EHR and EMR Differences: Understanding Key Distinctions
06 Dec 2025 By: Vlade Legaspi
Updated

Do you remember the times when you had to carry your health record files in a doctor’s office? These files were filled with lab results, notes, and all kinds of documents. It felt like going through the history of your entire health each time you flipped through that folder. But today, all that information is stored in a computer instead. That transition from paper records to digital ones is what has changed the whole healthcare system.
The thing is, this transition to digital records has also brought a lot of new terms with it, which are still quite confusing for people, such as EHR and EMR. Just by looking at the words, one might think that these terms mean the same thing. However, knowing what EHR and EMR differences are will help you understand less jargon if you are trying to find your way through the healthcare system.
What Exactly Are EMRs?
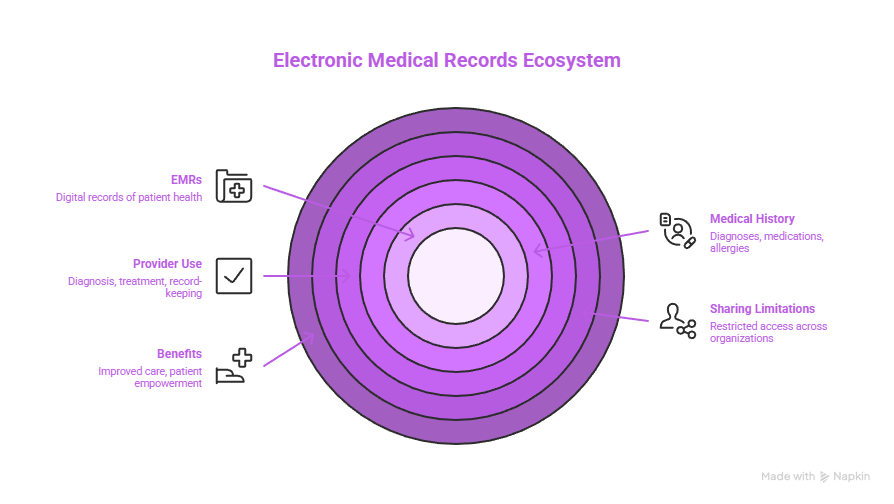
Electronic Medical Records go by the name EMRs most of the time. They work as digital copies of those paper files clinicians kept in their offices back in the day. You might picture them like a quick digital view of your health background tied to just one medical practice. That setup pulls in specifics such as diagnoses patients receive, medications they use, dates for immunizations, lists of allergies, and outcomes from lab work done at visits.
Providers turn to EMRs above all for handling diagnoses and treatments. The systems cut down on paperwork hassles and help doctors keep tabs on how patients improve as months pass. Even so, these records tend to stay narrow in reach. They focus on details from one healthcare spot or team only.
Take a trip to your regular doctor for instance. The EMR at that office holds every note and test finding from your time there. Things change if you end up with a specialist or in a hospital setting. Those other records stay out of reach unless staff share them on purpose. Limits like that create problems now and then. They leave holes in care because providers lack the whole story of a patients health when big choices come up.
Putting EMRs into place has shifted how medical staff handle tech in their daily work. Plenty of these systems pack in tools these days. You see reminders for routine checkups to catch issues early, warnings about drugs that could clash, and portals where people view their own health data directly. The move brings real gains in how care gets delivered with less waste. Patients gain more say too. They step up in watching over their own well-being.
Key Features of EMRs
- Contain medical and treatment history from one practice
- Used internally by providers for diagnosis and treatment
- Improve accuracy and efficiency of record-keeping
- Limited sharing capabilities across different healthcare organizations
Defining EHRs: More Than Just Digital Records

Electronic Health Records are more than just simple medical files. They take all the information from EMRs and develop them to provide a broader view of a patient’s overall health condition. Such systems are designed to be shared among different departments of healthcare. So, the data can be communicated without any hassle from one specialist to labs, hospitals, and in some cases, directly to the patient.
One of the biggest factors are interoperability. EHRs are instrumental in coordinating care from various sources. They prevent a situation where tests are repeated, the wrong medications are given, and the patient is missing steps in their treatment plan. Quite a few of them also connect with the features for monitoring public health trends, billing, and increasing the participation of patients. When the data of the patient is kept in one central location, the providers can easily access what they need in order to make the best decision. This usually results in better outcomes of the people who are getting care. Additionally, these records are a part of research and larger health initiatives. The data gathered from a large number of cases show the trends that influence policies in the future.
Imagine that you are rushed to the ER a day. The doctor who is available very quickly brings up your electronic health record to see your medical history, allergies, and what medications you are currently taking. That one quick look can be the rescue of your life in a moment of crisis.
Suppose you are allergic to penicillin and have a bad reaction to it? The doctor immediately finds the data and decides not to give it to you. That is the prevention of the occurrence of a disastrous situation. In addition, EHRs have the ability to determine that drugs can be combined only if certain conditions are fulfilled. That is why, the treatment remains safe and effective.
Core Characteristics of EHRs
- Comprehensive patient data from multiple providers and settings
- Designed for sharing and interoperability
- Support for clinical decision-making and care coordination
- Often include patient portals for direct access to health information
EHRs usually pack in smart analysis tools too. Providers use them to spot habits in how care gets given, follow results as time goes on, and even guess at risks ahead. This helps a lot with long-term illnesses. Keeping an eye on things and stepping in at the right moment improves how those conditions get handled. It raises the daily life quality for folks dealing with them. Patient portals add to that by letting people join in more. They see their own records, lab outcomes, and learning materials about their issues. That builds better understanding of personal health.
EHRs boost talk between patients and their care teams in important ways. Secure messages let people send questions, ask for more meds, or book visits without picking up the phone or showing up. It simplifies everything involved. At the same time, it builds stronger teamwork vibes with doctors and staff. As tech keeps changing, EHRs will open up even more ways to deliver care. They push toward treatments that fit each person better and work more smoothly overall.
Why the Confusion: EHR and EMR differences

People often mix up the terms EMR and EHR. Even folks in healthcare do it all the time. The overlap in what they do causes some of that mix-up. Plus, lots of systems out there don’t clearly separate the two.
EMRs came first when it came to turning patient records digital. They mainly aimed to swap out old paper charts. Then technology got better. The push for sharing info more easily grew too. That led to EHRs showing up as a fuller kind of setup. Some companies sell their stuff as both EMR and EHR. That just makes things even fuzzier.
It really counts to get these differences straight. They shape how providers handle patient data. They also affect how patients get their own info. Take a doctor’s office with just an EMR. They might struggle to send records to another provider. That could hurt the overall care you get.
EHR systems go way past simple record storage. They pack in tools for analyzing data. They handle population health too. Some even have ways to connect with patients directly. Providers can track how one patient does. They can spot patterns in big groups as well. That turns out super useful for health efforts on a wider scale. EMRs stick closer to just the medical details for each person. They don’t stretch as far into bigger healthcare pictures.
Rules around these techs add more twists. The HITECH Act kicked in with its rules. It nudged groups to pick EHRs that hit certain meaningful use marks. Adoption of EHRs jumped because of that. Still, the blur keeps going. Some EMR-labeled systems fall short on those standards. Providers and patients end up unsure about what their setups can really do.
How EMRs and EHRs Impact Patient Care
EMRs and EHRs both help make patient care stronger. Their effects differ though. It depends on how broad they are and what they offer.
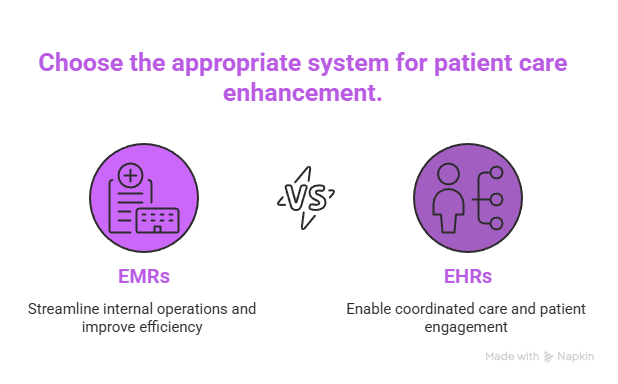
EMRs: Streamlining Internal Practice Operations
In one office, EMRs cut down on mistakes. They make writing notes faster. They let you pull up patient histories right away. That means diagnoses get more spot-on. Treatment plans improve too. For the staff, EMRs ease billing. They handle reports for rules as well.
EMRs stay inside that one place though. They can trap info in bubbles. A patient seeing different doctors means each has their own EMR. Sharing doesn’t always work smooth. Care ends up patchy because of it.
Putting in EMRs takes real money for training and gear. Workers need good lessons on using them. That can mess up daily flows for a bit. Once they settle in, EMRs boost how things run in the clinic. Pros spend less time on paperwork. They focus more on the people coming in. Grabbing past medical stories or old treatments quick helps tailor care better. In the end, that lifts patient results.
EHRs: Enabling Coordinated, Patient-Centered Care
EHRs work to bust those info traps. They pull together details from all over. You get a full picture of someone’s health that way. It leads to smarter choices in care. It stops problems like clashing meds or repeat tests.
Patients gain from EHRs with online doors to their stuff. They see lab results there. They book visits. They talk to their doctors too. That openness gets people more into their own treatment. They stick to plans better.
EHRs also link up care across providers. That’s key for long-term issues needing team input. Say someone has diabetes. They might see a hormone expert, a food advisor, and their main doctor. EHRs make sure everyone sees the latest facts. They team up well on the care outline. That link-up raises care levels. It builds trust too. Patients feel in the loop on their health path.
Regulatory and Privacy Considerations
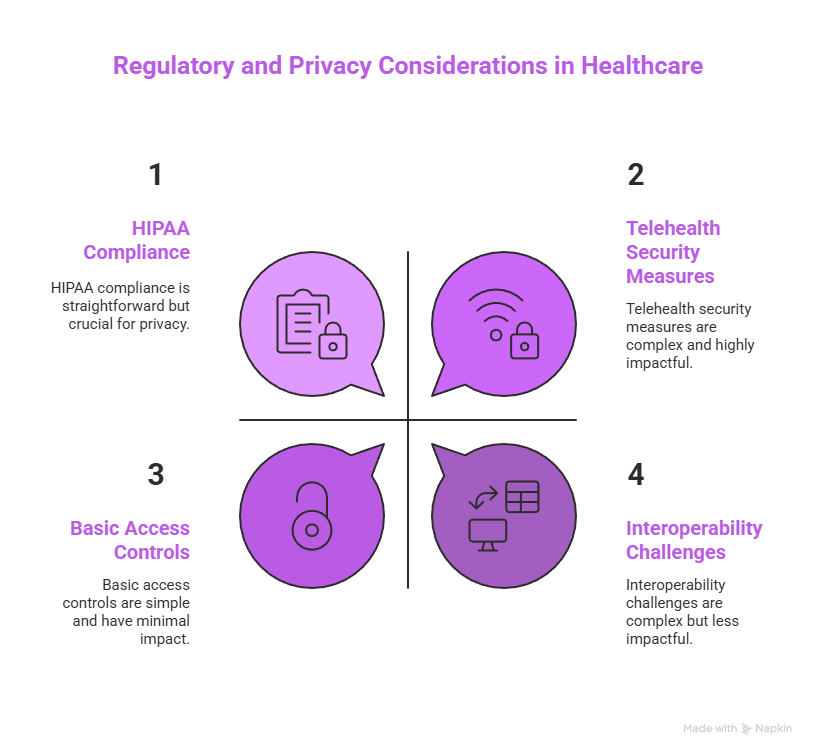
EMRs and EHRs both face tough rules. They guard patient privacy. They secure data tight. In the US, HIPAA lays out the basics for protecting medical details. It requires strong safeguards. It slaps fines for slip-ups. Bad cases can bring charges too. As tech changes, rules shift with it. New guides pop up for fresh risks and tools.
Providers have to set up locks like coding data. They control who gets in. They track changes. That holds for EMR or EHR setups. EHRs share across groups though. They need stronger ways to connect and stay safe. That sharing opens weak spots if handled wrong. Groups must keep up with top ways to protect. They train staff ongoing to spot dangers. Telehealth adds more hurdles now. Info zips over the web. That calls for even tighter security steps.
Patients ought to know their access rights to records. They should get how data moves and gets used. When providers explain handling clear, trust grows. People join in their care more. They can ask to fix wrong spots in records too. That’s big for keeping health info right. Knowing those rights lets patients step up in their health. It creates real teaming with providers. Healthcare keeps moving to put patients first. Informed okay and right use of data stay huge. Patients need to feel safe with their personal health details.

Choosing Between EMR and EHR Systems: What Providers Should Consider
Choosing the appropriate system is a matter of the size, patient population, and care coordination goals of the healthcare organization.
EMRs may be enough for small practices to internally manage patient information. They are a financially viable way to digitize records and elevate office productivity. For direct primary care (DPC) models, choosing a purpose-built DPC EMR or EHR can be especially valuable. These systems are designed to support smaller patient panels, long-term patient relationships, simplified billing structures, and direct communication between providers and patients. EMRs by allowing the office to run administrative tasks con amore such as appointment scheduling and billing can shorten the time that staff dedicate to paperwork thus freeing up their time for patient care. Moreover, EMRs have the ability to improve the accuracy of patient records hence, the possibility of errors due to illegible notes or poorly organized filing systems is minimized.
On the other hand, big practices, hospitals, and integrated health systems generally need EHRs to help complex workflows and sharing of information among departments and external providers. EHRs are not only the means to the management of patient data in all aspects but also the real, time access to medical histories, lab results, and imaging studies are made possible. The connectedness is vital to be sure that all healthcare providers who are part of a patient’s care have the latest information leading to better clinical decisions and enhanced patient outcomes.
Key factors in choosing a system include:
- Interoperability: Can the system exchange data with other healthcare entities?
- User Experience: Is the interface intuitive for clinicians and staff?
- Compliance: Does the system meet regulatory requirements?
- Patient Engagement: Does it offer portals or apps for patients?
- Cost and Support: What are the implementation and maintenance expenses?
The decision-making process has to take into account how well a system can scale up later on. Healthcare organizations often expand or shift their focus as time goes by. Their requirements end up changing quite a bit. They really need something flexible enough to keep pace with those shifts. Consider a small clinic just getting started. It could grow into several sites or branch out into new kinds of services. That would demand a tougher EHR setup to manage higher numbers of patients and a wider range of medical areas. Training and support stand out as key parts of the picture too. When staff get fully comfortable with the system, it runs more effectively and keeps users happier overall. Spending on solid training efforts builds up their skills and assurance. In the end, that creates an easier rollout and stronger day-to-day use of whatever option gets picked.
The Future of Health Records: Integration and Innovation
Healthcare tech keeps changing at a fast clip these days. The differences between EMRs and EHRs start to blur a little. Systems pull in more tools and work better with each other across the board.
New developments show up in areas like artificial intelligence for digging into health info. Blockchain handles record storage in a secure way. Mobile apps link right up to EHRs for easier access. All this points toward more tailored patient care and greater control for individuals involved. AI tools, for one, look at past records to forecast what might happen next. Providers can then adjust plans to fit each person’s situation. Blockchain, on the other hand, spreads out data handling without a central point. Records stay safe from changes and only open to those cleared for it. That builds more confidence in how things operate.
Government efforts and set standards push harder for sharing data too. The aim stays on boosting public health results while cutting down expenses. Everyone wants a smooth setup centered on the patient. This move goes beyond just the tech side of things. It builds ties between all the players, from doctors and insurers to the patients themselves. More groups follow common rules for swapping info. Real-time tracking of health issues picks up speed. Interventions happen sooner rather than later. Take telemedicine setups as an example. They tap into these links for quick check-ins and ongoing care. That improves how health gets handled and leaves patients feeling more content.
Trending Now!
An EMR (Electronic Medical Record) is essentially a digital version of the old paper charts doctors used to keep. One of the main features is that providers are able to keep track of patient information including medical history, treatments, medications, and lab results through these records, which are mostly limited to a single practice. EMRs can, in principle, facilitate faster and more accurate work, but they have not been developed in a way that would allow them to share data with other healthcare providers automatically. Thus, if a patient needs to see a specialist for a consultation or goes to another clinic, their data have to be duplicated in a hard copy, which can take more time and lead to a break in the continuity of the care process.
By contrast, an EHR (Electronic Health Record) is a level above. It contains as much patient information as an EMR, but the concept is that it can be shared among different healthcare providers. In other words, any authorized provider whether a hospital, lab, or specialist can access and update the patient’s info that is the most recent one. The aim of such a system is to facilitate better care coordination, quicker decision, making, and improved patient outcomes. In addition, EHRs give practices the opportunities to comply with value, based care requirements and enhance their productivity through features like automated documentation and real, time insurance verification.
Summary: Understanding EHR and EMR Differences Matters
EMRs and EHRs both hold important spots in today’s healthcare world. Yet they handle distinct tasks. EMRs act like digital paper files for one office only. EHRs create full records that move easily between various care spots. This split makes a big difference in recording, reaching, and using patient details among pros. EMRs usually hold treatment and medical pasts for folks in a single spot. They support routine work like booking visits and handling payments. EHRs focus on linking up across providers. Info flows without hitches, which helps a lot in urgent cases.
Grasping these points lets patients push for stronger care options. It also guides providers toward systems that match their setup. Patients who spot EMR limits might look for EHR users instead. Their history shows up fast for any expert they see. Health tech keeps advancing all the while. The emphasis falls on making data easier to reach, safer to store, and tied to better results for people. Cloud EHRs and phone-based health tools change delivery methods. Updates happen live, and checks occur from afar. These steps draw patients in more. Providers gain from fresh info to guide choices.
Do you wish to be the first one to adapt to new changes? Be a part of Helpsquad Health which is such a community where patients, providers, and healthcare innovators come together. We are sharing insights, tools, and updates that empower you to go through the ever, changing health tech realm with confidence.
What is the main difference between an EMR and an EHR?
The core difference between EMR and EHR is scope. An EMR (Electronic Medical Record) is like a digital version of a paper chart for one practice, it’s mainly used inside a single clinic or office to document diagnoses, medications, allergies, lab results, and treatment history. An EHR (Electronic Health Record) goes further: it pulls data from multiple providers and locations and is designed to be shared securely across hospitals, labs, and specialists, giving a complete, up-to-date view of a patient’s health. This is the practical EHR EMR difference people mean when they ask about the “difference EMR and EHR.” HelpSquad
How do EMR and EHR systems impact patient care in everyday healthcare settings?
EMR/EHR systems both improve care, just in different ways. EMRs help individual practices streamline documentation, reduce errors from handwriting, speed up note-taking, and support more accurate diagnoses and treatment decisions inside that single office. EHRs connect the dots across providers: they reduce duplicate tests, help avoid drug interactions, support team-based care for chronic conditions, and often include patient portals for messaging, appointments, and test results. Together, these EMR EHR systems support safer, more coordinated care and better patient engagement. HelpSquad
When should a healthcare organization choose an EMR instead of an EHR?
A healthcare EMR can be enough for a small, single-site practice that mostly treats patients in-house and doesn’t need to exchange a lot of data with external providers. EMRs are often more affordable, easier to implement, and still offer big gains in office productivity, like smoother billing, scheduling, and internal documentation. Larger practices, hospitals, and integrated health networks usually need an EHR instead, because they depend on real-time data sharing across departments and outside organizations to coordinate complex care. HelpSquad
Why do people (and even providers) still mix up EMR and EHR?
The terms get blurred for a few reasons. EMRs came first as basic digital charts, and EHRs evolved later as more advanced, interoperable systems. Many vendors market their products using both terms, and some EMRs have added limited sharing features that make the line feel fuzzy. On top of that, regulations like the HITECH Act pushed for “meaningful use” of certified EHR technology, but not every system labeled EMR or EHR fits neatly into one category. All this leads to ongoing confusion about EMR–EHR differences, even inside healthcare. HelpSquad
What privacy and regulatory rules apply to EMR and EHR systems?
Both EMRs and EHRs must protect patient data under strict privacy laws. In the U.S., HIPAA sets requirements for safeguarding health information, including access controls, encryption, audit logs, and breach reporting. Because EHRs are built for sharing data across organizations, they face extra scrutiny around secure connections and identity management. Telehealth and remote access add even more risk, so organizations need strong security policies, regular staff training, and up-to-date technical safeguards regardless of whether they’re using an EMR or an EHR. HelpSquad
How are EMR and EHR systems evolving with AI, mobile apps, and other new tech?
The line between EMR and EHR is getting blurrier as technology advances. Modern systems are adding AI tools to analyze large volumes of health data and predict risks, mobile apps that let patients and clinicians access records from anywhere, and even blockchain-style approaches for tamper-resistant data storage. EHRs increasingly connect with telemedicine platforms, remote monitoring devices, and public health systems, pushing toward more personalized, real-time, and patient-centered care. HelpSquad
Where does HelpSquad get the information for this article on EHR and EMR differences?
HelpSquad’s blog on EHR and EMR differences pulls from a mix of healthcare regulations, industry best practices, and reputable health IT sources they reference in the article (such as resources on EMR data-sharing limitations and HIPAA). It’s written by a HelpSquad marketing team member with experience in healthcare-related support services and was recently updated (December 2025), reflecting current trends in interoperability, telehealth, and emerging technologies. These sources and updates help keep the explanation accurate, practical, and aligned with how providers actually use EMR and EHR systems today. HelpSquad
How can patients tell if their provider uses an EMR or an EHR, and why does it matter?
Patients can look for a few signals. If your provider can easily share your records with other clinics, hospitals, or specialists and offers a portal where you can see your history from multiple sites, they’re likely using an EHR, not just an EMR. If records seem to stay “stuck” in one office and need to be faxed, printed, or repeated elsewhere, that suggests a more limited EMR setup. Understanding this difference EMR and EHR setup matters because it affects how smoothly your information follows you, how well your care team coordinates, and how likely you are to avoid repeated tests or medication errors. HelpSquad