How Does AI Reduce Costs in Healthcare: A Comprehensive Guide
15 Jul 2025 By: Vlade Legaspi
Updated
AI reduces spending by automating administrative paperwork and using predictive analytics to prevent expensive emergency room visits. If you are researching how does ai reduce costs in healthcare, it works by streamlining medical billing and managing hospital bed capacity more efficiently. For example, voice-enabled documentation tools can cut a doctor’s charting time by nearly fifty percent. This efficiency allows medical teams to focus on patient care while lowering the overall operational costs for healthcare systems.
Having managed clinical operations for years, I have seen how thin budgets can get when administrative waste goes unchecked. We reached a point where we couldn’t just work faster to save money; we needed smarter systems to help us manage the load. In this article, I will explain how does ai reduce costs in healthcare by focusing on real-world implementations that actually move the needle. I will walk you through a clear strategy for using these tools to protect your bottom line.
How Does AI Reduce Costs in Healthcare: Administrative and Workflow Automation
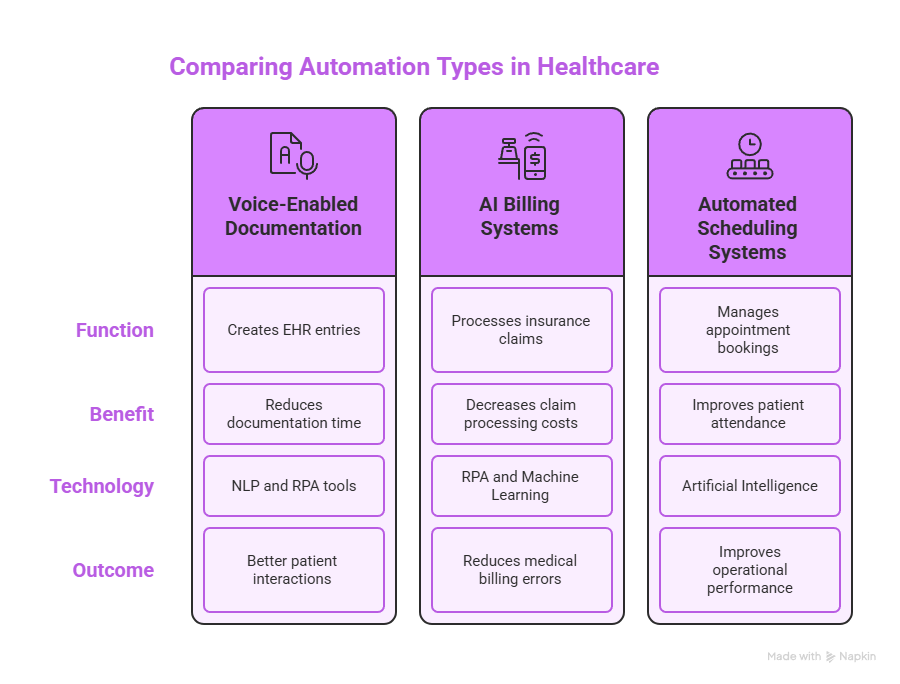
When I look at the numbers, I’m still struck by how much time and money gets eaten up by paperwork. A 2022 Annals of Internal Medicine study found that administrative costs make up about twenty-five percent of all healthcare spending in the U.S., and I see that every day in how teams work. When people ask me how does ai reduce costs in healthcare, I often start with what I’ve seen around admin work. The combination of natural-language processing (NLP) and robotic process automation (RPA) now handles a lot of those repetitive tasks that used to drain staff time. For example, voice-enabled documentation tools can turn a doctor’s spoken notes into automatic entries in the electronic health record. At the University of Kansas Health System, they tried out this pilot program. It brought down the documentation time for each patient visit from 16 minutes to just 9. That kind of change really helped doctors take on more patients. They felt less burned out too. Plus, they could put their energy into actually listening to folks instead of dealing with all those forms. The care process runs smoother now. Patients get a better experience overall. It happens simply because physicians stay more present right there in the room.
I’ve also watched AI tools become almost standard in many billing departments that are trying to clean up and speed up claims processing. RPA bots now run quietly in the background, checking insurance coverage, spotting missing information, and creating standardized claims before a human ever has to step in. One New England–based regional insurer reported a 30 percent drop in claim-processing costs in just six months after rolling out an AI-powered clearinghouse system. To me, that’s a clear example of how automating the right pieces of the workflow can directly cut workforce costs and accelerate the revenue cycle. On top of that, the machine learning models inside these systems keep learning from past claims, which helps them get more accurate and efficient over time. As these tools evolve, they’re starting to reduce medical billing errors too, something that can have a huge financial impact on both providers and patients.
Scheduling is another area where I’ve seen AI quietly reshape how things run. Automated scheduling setups are really shifting the way clinics and hospitals handle their appointment books. They grab patient details, check personal likes, and offer or set times that fit better for all involved. Take one healthcare spot in California. They put in an automated reminder setup. After that, patients showed up 25 percent more often. That’s not just a nice operational win, it means people are actually getting to their appointments on time and receiving the care they were supposed to get. The result is better use of staff time, fewer gaps in the schedule, and better health outcomes. As automation spreads through healthcare administration, I’m seeing more chances to improve both the patient experience and the overall efficiency of how care is delivered.
How Does AI Reduce Costs in Healthcare: Predictive Analytics for Hospital Operations
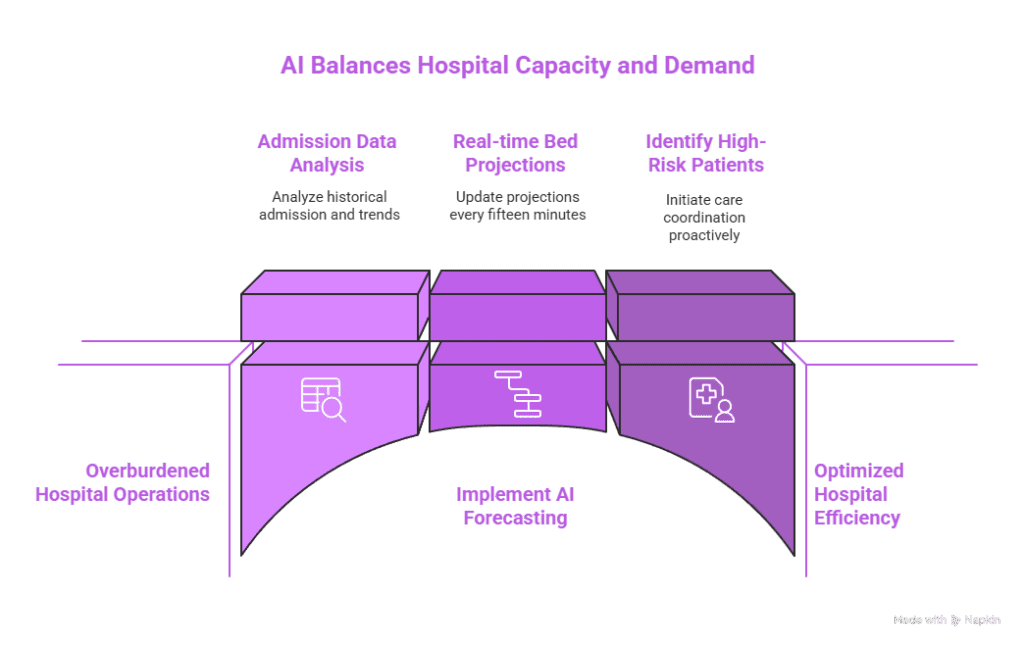
When I think about how does ai reduce costs in healthcare, one of the first things that comes to mind is bed management. I’ve seen how hospital expenses climb when beds sit empty, but things get just as expensive when wards are packed, staff rack up overtime, and patients end up being transferred to other facilities. It’s a tough balance to manage manually. That’s where AI tools have really started to make a difference in healthcare operations. By looking at historical admission patterns, local disease trends, and even weather data, these systems help hospitals match capacity with demand instead of constantly reacting in crisis mode. Take Johns Hopkins Hospital as one example. Their predictive setup there keeps updating projections on bed availability every fifteen minutes. In that first year of operation, it managed to reduce patient wait times by 38 percent. It also saved roughly twenty million dollars on overtime that really was not needed. That’s not a small tweak, that’s a structural change in how the hospital runs day to day.
I’m also very aware of the extra pressure that Medicare readmission penalties put on hospitals. Every avoidable readmission feels like both a clinical and financial failure. Machine learning models have become an important tool here: they flag patients who are at high risk of coming back, so teams can step in with better discharge planning, follow-up calls, or coordinated care. One North Carolina health system put this into practice with heart-failure patients and managed to reduce readmissions by 12%. That translated into about $4.3 million a year in savings from avoided penalties and uncompensated care. For me, these kinds of results make the answer to “how does ai reduce costs in healthcare” very concrete: it’s not just about cool tech, it’s about fewer rushed decisions, more proactive care, and real money saved while patients get better support.
How Does AI Reduce Costs in Healthcare: Clinical Decision Support and Diagnostics
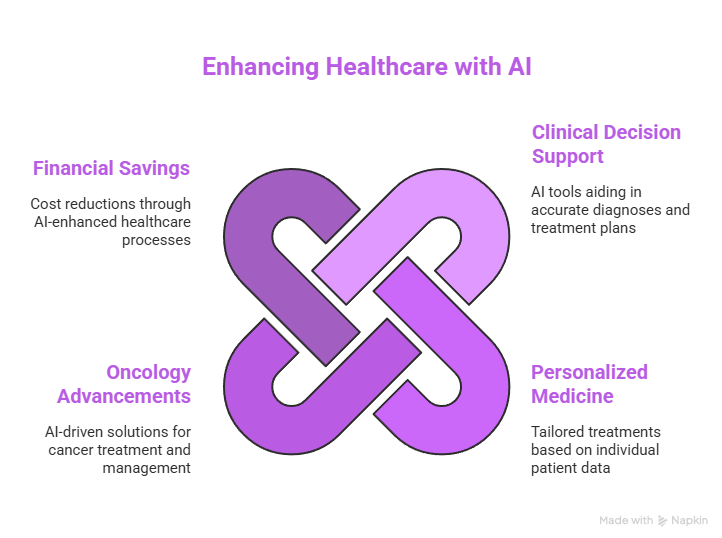
Whenever I consider the true human and financial costs of healthcare, I always end up dwelling on diagnostic errors. That covers things like getting the diagnosis completely wrong or missing a condition before it gets too far along. Those kinds of mistakes end up being hugely expensive. They hit hard in every possible way. One of the clearest answers to how does ai reduce costs in healthcare is through better, faster diagnostic support. Convolutional neural networks can now review medical images with accuracy on par with subspecialist radiologists, but at a scale no human could match, thousands of scans in an hour. A study in The Lancet Digital Health showed that AI tools improved mammography accuracy by 9% compared with traditional double-reading. That kind of lift doesn’t just look good on paper; it means more cancers caught earlier, when treatments tend to be less invasive, less costly, and more effective.
I’ve noticed how AI powered decision support systems really shift things once a diagnosis gets handed down. These systems grab data from lab tests and past medications along with the patient’s general health to come up with treatment options that fit better. Take Intermountain Healthcare for instance. Their tool for spotting sepsis cut mortality rates by sixteen percent. It also trimmed hospital stays down to about one point five days less for each patient. That kind of change added up to around six thousand five hundred dollars saved per hospital visit. Now spread those gains over thousands of patients. The money side of it piles up fast into millions. Lives get saved right alongside that financial boost.
When I talk about personalized and precision medicine, I often think about how much waste is baked into “trial-and-error” prescribing. Standard methods tend to push doctors into trying one medication after another on patients. This results in plenty of wasted drugs along the way. It also creates side effects that patients could have skipped entirely. On top of that, it leads to emergency room visits that turn out to be completely avoidable. Models powered by AI pull together genomic details with things like phenotypic traits and lifestyle factors. They help physicians get a much better sense of which patients will actually do well on certain treatments. Over at Cleveland Clinic, they put a pharmacogenomic algorithm to work. It cut down adverse reactions in heart patients by a solid 16 percent. At the same time, it shaved off roughly 2.1 million dollars from yearly pharmacy expenses.
Oncology really stands out as a key example of this whole shift. Clinicians at Memorial Sloan Kettering Cancer Center depend on AI tools for matching those in-depth tumor profiles to the most appropriate drug treatments. This setup really helps them reduce the number of chemotherapy rounds. It also spares patients from enduring a bunch of those tough side effects. The payoff isn’t only clinical, between lower drug spending and fewer complications to manage, the annual savings exceed $8 million. For me, these kinds of results make it very clear: when we ask “how does ai reduce costs in healthcare,” the answer is tied directly to more precise diagnoses, smarter treatments, and fewer avoidable downstream problems for both patients and providers.
How Does AI Reduce Costs in Healthcare: Drug Discovery and Trial Optimization
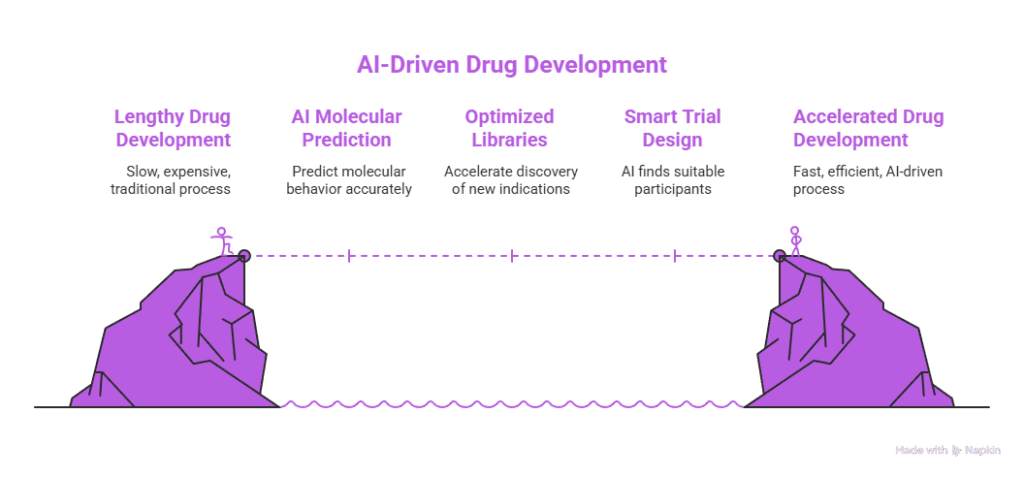
When I think about the long, expensive road of drug development, it’s easy to see why so many people ask how does ai reduce costs in healthcare. A traditional drug development cycle can easily stretch over ten years and cost up to $2 billion before a new therapy reaches patients. What I’ve seen with AI is that it can compress several of those stages by predicting molecular behavior, optimizing compound libraries, and surfacing new indications much faster than conventional methods. One example that really stands out to me is a London-based biotech that partnered with a U.S. pharma company: they used deep-learning models to design a novel fibrosis candidate that reached Phase I trials in just twelve months. That effort cut early-stage research costs by about 70% and brought the timeline down to roughly a quarter of what we’d usually expect.
At the same time, I’ve watched research teams bring in OEE software to keep a closer eye on how lab equipment is actually being used. By tracking utilization and flagging bottlenecks in workflows, they’ve been able to squeeze more throughput out of the same instruments during intense screening phases instead of constantly pushing for more hardware. On the financial side, a lot of biotech organizations I’ve worked with are now leaning on AI-powered biotech accounting tools and biotech accounting software to handle cost tracking, grant management, and complex reporting. Those platforms give real-time visibility into R&D spending and make sure money from different funding sources is allocated correctly. For me, that combination, faster science, more efficient lab operations, and tighter financial oversight, is a big part of how AI helps maintain financial integrity while still accelerating innovation.
Smart Clinical Trial Design
When I look at clinical trials, one of the biggest headaches I see over and over is recruitment and retention. Finding the right participants and keeping them engaged is incredibly expensive and time-consuming. When people ask me how does ai reduce costs in healthcare, I often point to this exact problem. AI tools can scan electronic health records to spot patients who match complex inclusion and exclusion criteria, automatically check their eligibility, and even flag where we’re likely to run into enrollment challenges before they happen.
I’ve come across this in actual practice. The Stanford Center for Clinical Research ran a cardiovascular trial that leaned on an AI system for recruitment support. Once they implemented it, the researchers completed enrollment six months early. They also cut operational costs by roughly three million dollars. For me, that’s a clear example of how smarter, targeted recruitment doesn’t just speed up the science, it also takes a meaningful bite out of trial expenses.
How Does AI Reduce Costs in Healthcare: Chronic Disease Management and Remote Monitoring
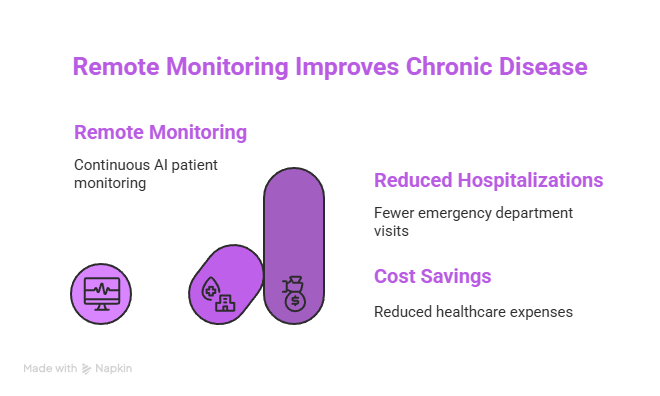
When I step back and look at spending patterns, it’s clear that most healthcare costs are driven by chronic conditions like diabetes, heart failure, and COPD. One of the most practical answers to how does ai reduce costs in healthcare is through continuous remote monitoring. AI-powered systems that track patients at home let care teams spot early signs of trouble and adjust treatment plans before someone ends up in the hospital. I’ve followed the virtual cardiac rehab program at Kaiser Permanente, which uses wearable sensors and machine-learning models to flag irregular heart rhythms. Since they rolled it out, emergency department visits among enrolled patients have dropped by 27%, opening up bed capacity and generating an estimated $11 million in annual savings.
I’ve also seen how small, everyday “nudges” can make a big financial difference. Smartphone apps for tracking glucose levels go beyond simple charts and visuals. They provide actual tips on food choices and timely alerts for medications. This type of help cuts down on low blood sugar incidents. In the end, that leads to less need for emergency transport or hospital visits. In a similar way, practical choices at home—such as using the Best juice jars for cold-press juicing to prepare consistent, portion-controlled drinks—can support healthier routines that are easier to maintain day to day.Overall, it benefits everyone involved. Costs for urgent care drop, and patients end up with stronger health over time. They gain a real sense of managing their condition better.
How Does AI Reduce Costs in Healthcare: Supply Chain and Inventory Optimization

When I look at hospital budgets, I’m always surprised by how much money quietly slips away through supply management, especially with surgical sutures and high-cost implants. It’s one of those behind-the-scenes areas where the answer to how does ai reduce costs in healthcare becomes very real. AI-based demand-sensing platforms can now analyze procedure schedules, supplier lead times, and historical consumption patterns to recommend precise reorder points. I’ve seen this in action at a 500-bed hospital in Chicago that implemented a demand-sensing platform and cut its medical-supply inventory value by 23%. That shift freed up about $5 million in working capital, without compromising patient care.
When I look at hospital budgets, I’m always surprised by how much money quietly slips away through supply management, especially with surgical sutures and high-cost implants. It’s one of those behind-the-scenes areas where the answer to how does ai reduce costs in healthcare becomes very real. AI-based demand-sensing platforms can now analyze procedure schedules, supplier lead times, and historical consumption patterns to recommend precise reorder points. I’ve seen this in action at a 500-bed hospital in Chicago that implemented a demand-sensing platform and cut its medical-supply inventory value by 23%. That shift freed up about $5 million in working capital, without compromising patient care.
On top of everything else, computer vision tools are really transforming the way organizations handle tracking and managing expiration dates. These setups move away from old manual inspections. They automatically keep watch on products instead. They spot items getting close to their expiration. They even kick off recalls whenever that becomes necessary. Hospitals end up catching problems well in advance this way. They steer clear of unnecessary waste. They also avoid those risky liability expenses down the line. Plus, they do not find themselves rushing to toss supplies at the very last second. Even worse, they prevent the mistake of putting outdated products to use by accident. For me, this is another clear example of how smart, targeted use of AI turns operational blind spots into real financial savings. For me, this is another clear example of how smart, targeted use of AI turns operational blind spots into real financial savings.
How Does AI Reduce Costs in Healthcare: Fraud, Waste, and Abuse Detection
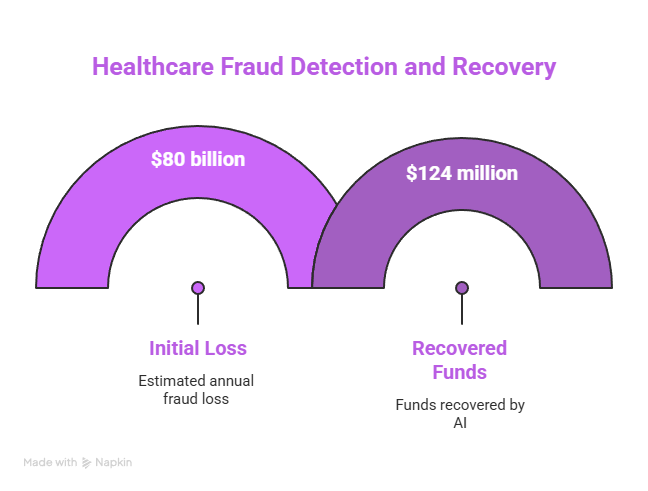
When people ask me how does ai reduce costs in healthcare, I often point to fraud detection as one of the clearest examples. The National Health Care Anti-Fraud Association estimates that fraudulent and abusive practices drain at least $80 billion from the U.S. healthcare system every year, and I’ve seen how painful that loss can be for payers, providers, and patients. Machine learning systems help by scanning claims data in real time, flagging suspicious billing patterns that would be almost impossible for humans to catch at scale. Blue Cross Blue Shield of Illinois, for instance, used an AI framework to uncover hidden up-coding schemes that traditional rule-based systems missed and recovered about $124 million in just the first eighteen months. That’s a huge impact from simply looking at the same data with smarter tools.
I’ve also watched intelligent document analysis change how audits get done. Auditors no longer need to manually go through every single detail one by one. AI tools handle the matching of patient records, clinical notes, and billing codes all automatically. This setup lets potential issues come up much faster than before. Cases turn out easier to look into as a result. Disputes get settled in less time overall. In practical terms, that reduces the need for drawn-out legal procedures and lowers the associated costs. To me, this is another powerful piece of the answer to how does ai reduce costs in healthcare: it doesn’t just find fraud, it streamlines the entire process of proving and resolving it.
How Does AI Reduce Costs in Healthcare: Challenges and Considerations
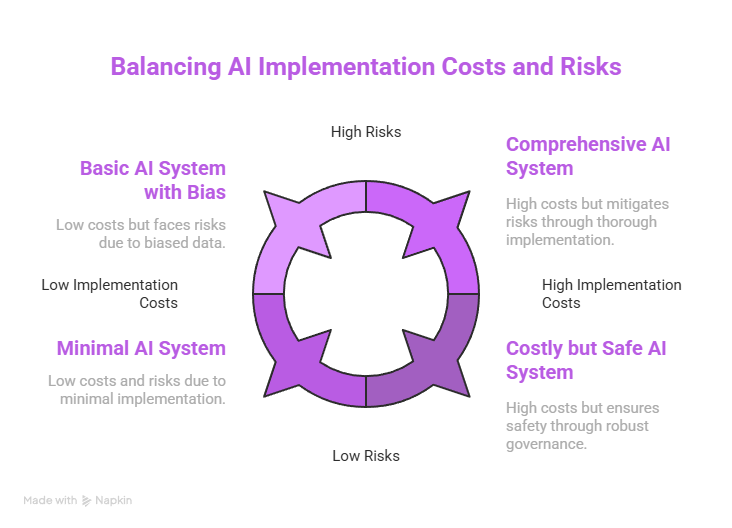
Whenever I talk about how does ai reduce costs in healthcare, I always feel the need to add a reality check: the savings don’t come for free. The potential is huge, but so are the upfront investments. In my experience, organizations have to pour serious money into data infrastructure, staff training, and system integration long before they see any financial return. Deloitte estimates that enterprise AI solutions can cost hospitals anywhere from $500,000 to $3 million just to get off the ground, and that means the real payoff often only shows up over several years, not a few months.
I’ve picked up that nothing in this area really clicks without solid, unbiased data to work with. Training data that tilts toward particular groups of people can make AI systems accidentally deepen the gaps in health care that already exist. This goes beyond just hurting individual patients in real ways. It often results in bigger expenses later from efforts to fix problems, hits to reputation, and potential legal battles too. For that reason, I view robust governance as something you cannot skip. Things like straightforward oversight, algorithms open to review, and checks from outside sources have to be built right into any meaningful AI effort. Lacking those protections means the tools designed to trim costs could wind up sparking fresh hazards and added outlays pretty much right away.
How Does AI Reduce Costs in Healthcare: Strategies for Successful AI Adoption
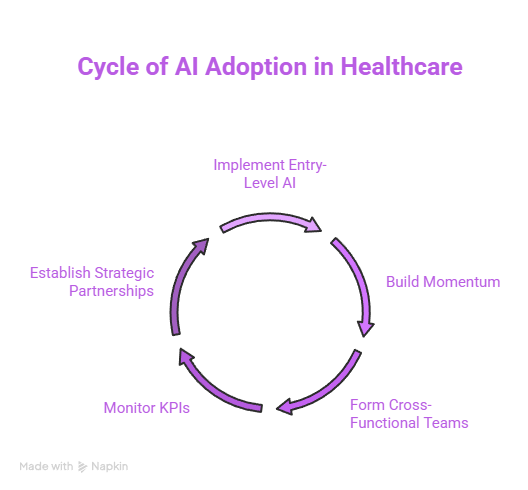
From what I’ve seen, rolling out AI in healthcare works best when it’s done gradually rather than all at once. That’s a big part of how does ai reduce costs in healthcare in a realistic, sustainable way. Starting out with those lower risk but high impact use cases makes a lot of sense for organizations. Things like automated appointment reminders or systems that predict claims denials let them test the waters without messing up the whole operation. These initial efforts bring in some fast successes. They also help save a bit of money right away. Plus they build up that internal trust and even secure more budget to tackle tougher clinical projects down the line.
I have picked up that all of this really needs collaboration across different groups. Implementing standards for clinical work and regulations works best when data scientists team up closely with clinicians. IT folks and compliance experts join in too. Each person brings their own part to the overall picture. To stay on course I make sure to check key performance indicators pretty often. Stuff like how long patients stay in the hospital readmission rates and cost per claim all matter a lot. Tracking these numbers as time goes on shows if the AI projects truly add value. They do not just look good in reports without real results. Many organizations now pair these efforts with AI finance tools to monitor costs, forecast ROI, and keep spending aligned with long-term financial goals.
Partnerships and Ecosystems
From my experience, no single organization can realistically build every AI algorithm it needs on its own. When I think about how does ai reduce costs in healthcare at scale, I immediately think about partnerships. Working with academic centers, technology vendors, and startup incubators not only speeds up innovation but also spreads out the risk. I’ve seen payment models where vendor fees are tied directly to verified cost savings, so everyone has skin in the game and a clear incentive to deliver measurable financial and clinical results.
TRENDING NOW!
Healthcare institutions experience increasing costs while doctors face excessive workloads and patients must endure extended waiting periods. AI technology provides a solution which enhances medical care while reducing expenses. The U.S. healthcare system can potentially save $150 billion annually through the implementation of AI tools including robotics and automation and Gen AI. The adoption of AI technology requires significant financial investment. The expenses for AI implementation depend on three main factors which include model complexity together with infrastructure requirements and data processing needs. The cost of a basic AI model reaches $40,000 but GANs and other advanced models exceed $200,000 in price. The selection between cloud-based and on-premises and edge AI infrastructure systems determines how costs will be distributed while affecting security measures and scalability capabilities. The total price increases due to data preparation requirements andEHR integration as well as compliance needs.
The initial cost of off-the-shelf AI solutions is lower but users must pay license fees while custom AI models can reach prices up to $500,000. ITRex demonstrates that actual model prices for telehealth and cancer care and eye treatment applications fall between $100,000 and $160,000. The implementation of AI technology results in reduced readmissions and automated tasks and enhanced accuracy which produces substantial financial savings. Healthcare providers need to factor in continuous expenses for retraining personnel and maintaining compliance standards and infrastructure maintenance. The implementation of open-source tools and readiness assessments together with small-scale starts help organizations reduce risks while improving their return on investment.
Conclusion
The healthcare value chain generates real and measurable cost savings through artificial intelligence systems which operate from billing offices to patient care settings. AI systems free up healthcare resources through automated tasks and decision support and operational prediction and waste elimination so organizations can invest in patient care. Institutions that handle their AI adoption process with care and handle data governance directly and focus on vital use cases will obtain the highest benefits. Responsible AI deployment enables both financial balance sheet improvements and better health outcomes for communities.
We at HelpSquad health is ready to help. Our trained virtual assistants and 24/7 support team handle healthcare tasks with ease. With bilingual agents from $9/hr. you get expert help without high costs.
FAQ’S
How does AI actually reduce costs in healthcare on a day-to-day basis?
AI reduces costs by making hospital operations and clinical decisions more efficient. In the article, you see AI used for bed management, predicting admissions, and aligning staff levels with demand so hospitals avoid both empty beds and expensive overtime. AI also flags patients at high risk of readmission, supports more accurate diagnoses, and suggests better-fit treatments. All of this cuts avoidable hospital days, penalties, and wasted treatments while improving patient outcomes.
How much can health systems save with AI assistants and other AI tools?
Savings vary by organization, but the article highlights several real-world numbers. Johns Hopkins saved about $20 million in overtime in the first year of using AI for bed and capacity management. A North Carolina health system saved roughly $4.3 million annually by reducing heart-failure readmissions. Blue Cross Blue Shield of Illinois recovered around $124 million in 18 months through AI-driven fraud detection. At a system level, the article notes estimates that AI (including robotics, automation, and Gen AI) could unlock around $150 billion in annual savings for the U.S. healthcare system.
What are the top AI solutions for reducing healthcare costs across the value chain?
The article points to several high-impact categories of AI for healthcare cost saving:
Operational forecasting and bed management to reduce overtime and transfer costs.
Clinical decision support and diagnostics (e.g., AI for imaging and sepsis detection) to catch disease earlier and shorten hospital stays.
Personalized and precision medicine to avoid trial-and-error prescribing and reduce adverse drug reactions.
Drug discovery and smart trial design to shorten development timelines and cut recruitment costs.
Chronic disease remote monitoring to prevent avoidable ER visits and admissions.
Supply chain optimization and computer vision inventory tracking to lower inventory value and waste.
Fraud, waste, and abuse detection to recover money lost to improper billing.
AI assistants and virtual support teams (like HelpSquad’s 24/7 agents) to offload routine administrative and patient-support tasks at a lower cost than traditional staffing.
How does AI help lower costs in chronic disease management and remote monitoring?
For chronic conditions such as diabetes and heart failure, AI systems continuously monitor patients at home and flag early warning signs before they escalate into emergencies. The article describes a virtual cardiac rehab program at Kaiser Permanente that uses wearable sensors and machine-learning models to detect irregular heart rhythms. Since implementation, emergency department visits dropped by 27%, freeing up bed capacity and generating about $11 million in yearly savings. AI-powered apps for glucose tracking also nudge patients on diet and medication timing, reducing expensive hypoglycemic events and avoidable hospital trips.
How can AI cut the costs of drug discovery and clinical trials?
AI shortens the long, expensive drug development pipeline by predicting how molecules will behave, optimizing which compounds to test, and finding new indications faster than traditional methods. The article cites a London-based biotech that used deep learning to design a fibrosis drug candidate that reached Phase I in about 12 months, cutting early-stage research costs by roughly 70%. In clinical trials, AI scans electronic health records to find eligible patients quickly and anticipate recruitment bottlenecks. At Stanford, an AI-supported cardiovascular trial finished enrollment six months early and reduced operational costs by around $3 million.
What are the main benefits and challenges of AI in healthcare?
On the benefits side, the article highlights: fewer diagnostic errors, shorter hospital stays, reduced readmissions, lower drug and supply spending, better chronic disease control, and major savings from fraud detection and automation. These are the core benefits and challenges of AI in healthcare that leaders weigh. The challenges include high upfront investment (enterprise solutions often cost hundreds of thousands to several million dollars), the need for robust data infrastructure and integration with EHRs, ongoing training and compliance costs, and serious risks if data is biased. Without strong governance and oversight, AI can deepen inequities and create new legal, reputational, and financial risks.
What are the pros and cons of AI in healthcare specifically for cost saving?
Pros:
– Automation of routine tasks (scheduling, claims, basic support) at a lower marginal cost.
– Better forecasting, which cuts overtime, unnecessary admissions, and inventory waste.
– More accurate diagnostics and personalized treatments that prevent costly complications.
– Stronger fraud detection, leading to recovered revenue and fewer abusive billing patterns.
Cons:
– Significant upfront spend on models, infrastructure, integration, and training.
– Ongoing costs for maintenance, monitoring, and regulatory compliance.
– Potential for biased algorithms, which can drive unequal care and costly downstream fixes.
– Operational risk if AI tools are implemented too fast, without clinician and IT alignment.
– Overall, the article suggests the pros and cons of AI in healthcare tilt strongly positive when organizations start with targeted, high-value use cases and manage governance carefully.
Where does this article get its information about AI healthcare cost savings?
The article grounds its claims in a mix of peer-reviewed research, real-world health system implementations, and industry analyses. It references outcomes from institutions like Johns Hopkins Hospital, Intermountain Healthcare, Cleveland Clinic, Memorial Sloan Kettering, Kaiser Permanente, and the Stanford Center for Clinical Research, as well as payers like Blue Cross Blue Shield of Illinois. It also cites estimates from organizations such as Deloitte, the National Health Care Anti-Fraud Association, and vendors like ITRex for AI implementation costs and model pricing. Together, these sources are used to show that cost savings from AI are not just theoretical—they’re already being measured in millions of dollars across diverse healthcare settings.


