How a Virtual Assistant for Mental Health Practices Transforms Care
14 Jul 2025 By: Mary Dellosa
Updated
Talk about anxiety, depression, PTSD, and burnout has gone from quiet talks to big headlines. The WHO reports a 25% rise in these issues during COVID’s first year. In the U.S., over 150 million people live in areas without enough mental health pros. This gap has sparked a push for new care options. One growing solution is a trained virtual assistant for mental health practice. They help extend a therapist’s reach, make care more personal, and handle simple tasks. This keeps the therapist at the center while making care faster and easier to get.
The Urgency of Innovative Mental Health Support
Even before COVID, getting mental health help was hard. In 2019, many waited weeks. That’s a long time when even getting up feels hard. Some days, you just need someone to see you and say, “I care”. In small towns, it’s even harder. Help is far, and it feels like no one sees what you’re going through. That’s why care that puts people first isn’t extra, it’s something we all need.
Young people are changing how we get help. Most Gen Z would try a mental health app before seeing someone in person. They grew up with phones, and online help feels safer and more private. It’s often the first step when asking for help feels hard.

By having virtual assistants, care can come to where people are, on phones, tablets, and laptops. That gives therapists more time to help with serious issues.
Apps like Calm and Headspace give easy tools like breathing and calming talks, even playlists that people use as music therapy programs. Some even have real people to guide you when things feel hard. These tools let people choose what feels right. Whether it’s an app or a helper to talk to, it gives back control when life feels out of control.
Many apps now track your moods and habits to give better advice. That means the help can fit your needs, not just follow a set plan. As more people use these tools, getting care feels easier, more personal, and closer to home.
What Defines a Virtual Assistant for Mental Health Practice?
A virtual assistant for mental health practice is a trained person who chats with users, collects info, handles tasks, and offers support. They may work on clinic websites, apps, or voice tools linked to health records. They often share tips like mindfulness reminders.
They follow strict health rules and keep data safe with encryption and access limits. Clinicians guide them to make sure they give the right kind of help. When utilized well, they help sort needs, handle admin work, and support users, without taking the place of a real therapist.
What are the Key Benefits for Clinicians and Clients?
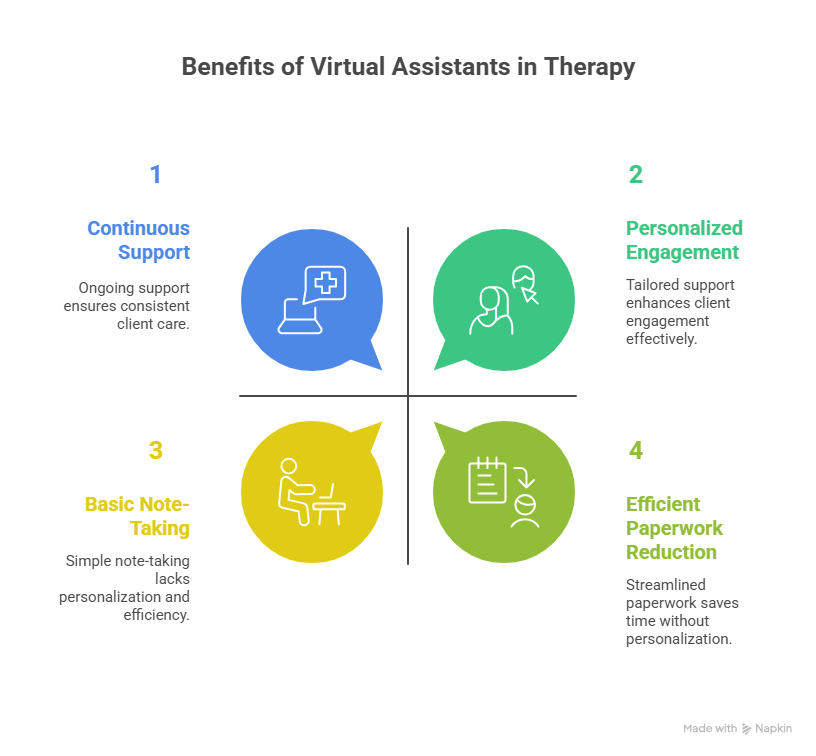
Efficiency and Accessibility
Therapists spend a lot of time on paperwork. One study found they use 31% of each session just on notes. Virtual assistants can cut that time. They transcribe talks, spot key themes, and prep progress notes.
This helps therapists meet rules without losing time. That saved time can go back to helping people or caring for themselves.
Personalization Without Compromise
People need different kinds of support. Virtual assistants can adjust based on your mood, answers, and past chats. These personal nudges help people stay engaged and feel seen. A 2022 study found they boost follow-through by up to 30%. And they do it without adding more work for the therapist.
Continuous Support and Early Escalation
A therapy session covers just 4% of a client’s week. Virtual assistants help fill the other 96% with check-ins, learning tools, and support prompts. If someone types worrying words, like thoughts of self-harm, the system can alert a therapist or guide the person to emergency help right away.
This safety net keeps care going between sessions and helps stop things from getting worse.
Practical Applications in Therapy Workflows
Success starts with using the right tech for real clinic needs. Intake is a strong first step. Instead of paper forms, a virtual medical assistant collects symptoms, background, and insurance info. They upload it straight to the clinic system.
This cuts front-desk time. Some clinics saw 40% fewer intake calls after adding virtual assistants. During care, virtual assistants send weekly check-ins by text or voice. Clinicians get alerts when scores change a lot, helping them focus sessions. Fewer missed visits means better care and stronger clinic income.
Addressing Privacy, Ethics, and Trust
A virtual assistant for mental health practice knows how to listen with care, offering support when someone feels alone or lost. They hear hard truths: stories of fear, trauma, shame, and hope. That trust is deep. Breaking it doesn’t just risk rules, it hurts real people.
That’s why privacy must be sacred. Virtual assistants follow laws like HIPAA and GDPR, use secure systems, and always get clear consent. Clinics owe it to both clients and assistants to check safety, ask hard questions, and make sure everyone is protected.
They should always have access to real-time human backup and clear info about who’s helping them. And we must guard against bias. virtual assistants work best when they reflect all voices, all backgrounds, all stories.
The best teams now open their systems to review, share fairness reports, and keep growing. Because it’s care. And care should always feel human.
How Do You Integrate Virtual Assistants Into Existing Practices?
Change is hard. A great tool only helps if people actually use it. That’s why rollout needs a smart, steady plan. Start small. Try virtual assistants with simple tasks first, like sending reminders. This gives staff time to learn and spot any issues.
Use feedback to fix problems before adding more features. Step by step works better than all at once. Training is key. Many therapists fear that tech will make care feel less human.
But showing how assistants cut paperwork and help with follow-ups can ease those fears. Sharing client stories about getting support anytime also helps show this is a team effort, not a replacement.
Technology must also work well with current tools. If data doesn’t move easily between systems, time gets wasted. Most virtual assistants now use standard technology that connects with health records and telehealth tools. That keeps everything running smooth.
Trending Now
Burnout is an extensive and major problem that mental health professionals face. It is mainly characterized by three features: emotional exhaustion, depersonalization, and feeling of no personal accomplishment. As a result, it can harm the individual’s well-being, the organization’s effectiveness, and the quality of the care provided. Although the rates of burnout are very high (21 to 67% depending on the study) and its consequences are serious (for instance, health problems, dissatisfaction with the job, high turnover, and poor service quality), the issue of burnout has not been given much attention in mental health settings. Only a few intervention studies have been conducted, and the results have been mixed, often originating from Europe and generally focusing on inpatient staff.
Cognitive-behavioral training, mindfulness, and the organizational changes concerning workload, supervision, and communication have been considered the most effective strategies. Nonetheless, in the case of the studies supporting the effectiveness of these approaches, the methodological problems like limited sample size and no long-term follow-up have somewhat weakened their findings. The authors insist on the urgent necessity for robust, multi-tier interventions that integrate both the individual and the system approaches, with the preventive and restorative components incorporated, and they also demand more extensive longitudinal research in order to enhance the situation for both caregivers and those whom they are serving.
The Future Landscape
Virtual assistants are growing more advanced. New tools can read tone in your voice and adjust responses based on how you feel. By combining voice, text, heart data, and behavior, virtual assistants now offer more personal, full support.
Need extra help for your team and your clients? HelpSquad Health’s virtual assistants take care of the small stuff, so you can focus on what matters most. Ready to make care easier, faster, and more personal? Let’s talk.
What is a virtual assistant for mental health practice?
A virtual assistant for mental health practice is an individual with a professional training who communicates virtually to provide assistance to both therapists and clients. Their role includes client interaction, data capture, appointment scheduling along with reminders, documentation support, and provision of tools such as mindfulness prompts, all these activities are strictly under clinical guidelines. They take the place of a therapist without driving out the need for real human care.
How do virtual assistants help with access to mental health care?
Virtual assistants provide support by making the service more accessible especially when there are not enough local providers or the waitlists are too long. They are available on clinic websites, apps, or messaging tools so that people can easily ask questions, fill in their details or receive support from their phone or laptop. This is particularly the case for Gen Z and others who are more inclined to use digital tools first before going for the traditional in-person care.
What are the ways in which virtual assistants help therapists’ workload and burnout?
Virtual assistants are a great support to therapists’ workload and they help minimize burnout. Therapists’ engagement with notes, forms, and admin is time-consuming which could account for a third of a session dedicated to documentation alone. Now, however, by the mental health practice virtual assistant, the therapist gets a coworker who can take care of the session transcription, theme extraction, making progress notes, and scheduling activities. In this way, the therapist can spend more time on clinical practice, have more space for self-care, and the likelihood of burnout happening is reduced significantly.
In what way do virtual assistants enhance the personalization aspect of mental health care over to the other side?
By sending messages that are not the same for every client, virtual assistants can tweak their messages according to a client’s current emotional state, objectives, and replies he/she has given in the past. They can personalize the offering of check-ins, whole practices along with reminders and resources which are in line with the individual’s mood. Research has confirmed that such support will be even more engaging and result in higher therapy attendance without taxing the therapist’s time.
Can bringing down therapists to look onto virtual mental health assistants?
No. Virtual assistants for mental health practices have been created to aid licensed professionals while not taking their place. They take care of tasks such as intake, follow-ups, simple questions, and between-session support whereas therapists take care of assessment, diagnosis, and treatment. When virtual assistants detect hazardous language or risk signals, they refer the matter to a human clinician or direct the person to get live help.