AI in Primary Care: Transforming Diagnosis, Treatment, and Patient Experience
11 Aug 2025 By: Vlade Legaspi
Updated
AI in primary care is used to improve diagnosis, personalize treatment, and make visits smoother by helping clinics triage patients, automate routine admin work, and support shared decisions without replacing the clinician. It can route patients to the right level of care, send reminders and education, flag high-risk patients after discharge, and suggest possible diagnoses when symptom patterns look concerning. For example, an AI triage tool can prioritize a patient with chest pain for urgent evaluation while directing a mild cold to self-care guidance.
Improving the Patient Experience
Patient experience is a central measure of primary care quality. AI has the potential to reduce wait times, improve access, and make communication more convenient. However, benefits depend on thoughtful design and sensitive implementation that preserves privacy and builds trust.
Access and Triage
AI-enabled triage systems can route patients to the right level of care — self-care resources, nurse triage, virtual consults, or urgent in-person visits. By prioritizing cases based on clinical risk, clinics can allocate appointments more effectively, shorten wait times for urgent needs, and reduce unnecessary emergency department visits.
Patient Communication and Education
The delivery of medication reminders and appointment scheduling and educational content happens through chat-based assistants and automated messaging platforms. The delivery of personalized and timely information helps patients follow their care plans and recognize when they need medical attention. The system requires human oversight and escalation pathways to prevent automated communications from missing important contextual cues that need clinician input.
Shared Decision-Making and Behavioral Support
Use in clinics needs strong data, clear models, and smooth fit in work flow. Bias or missing data can harm care, so tests on all groups and checks for change are key. Showing what drove a choice and giving confidence scores helps doctors know when to trust or dig deeper. AI must fit into records, give help at the right time, cut alerts, and note why it was used for safety and care records.
Training doctors and talking with patients are both vital. Doctors need to read results, see limits, and use AI for shared choices. Clear talks on AI’s role—gains, risks, and data safety, help trust and consent. With strong rules, checks, and doctor oversight, AI tools can boost speed, fairness, and accuracy.
Behavioral health is a strong use case. AI tools can spot mood, stress, drug use, and memory loss early by reading forms, notes, and device data. They can help teams match care, self-help, short talks, or a mental health expert, and track progress with tips or drug advice fit to the patient’s history.
Equity, privacy, and patient buy-in are vital in AI care plans. Model checks by group can stop gaps, and teams should be open on data use and give control to patients. Tools with shared choice prompts, culture-fit content, and many language options raise trust and success for all.
Implementation Strategies for Practices
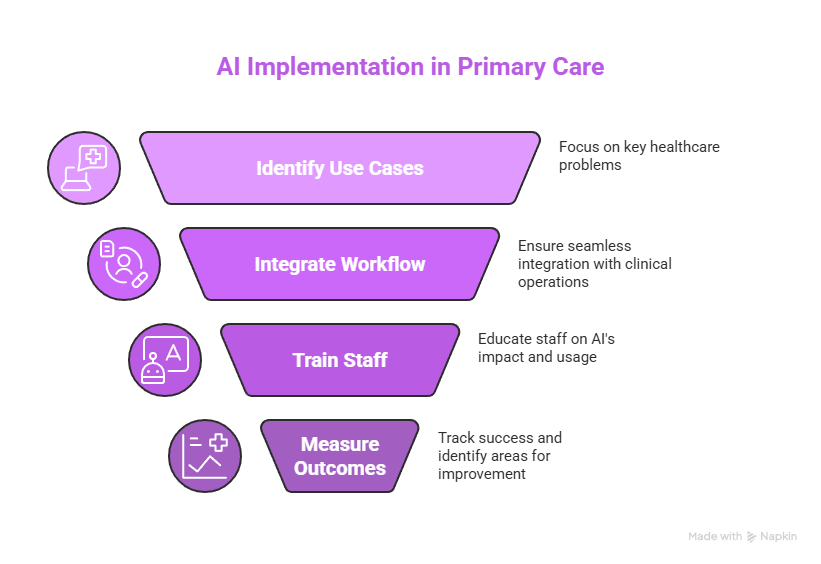
The successful implementation of AI in primary care requires strategic planning together with clinician participation and ongoing assessment. The following strategies help ensure technology augments care delivery effectively.
Start with Clear Use Cases
The first step should focus on applications which address major healthcare problems or deliver quantifiable efficiency improvements through documentation automation and abnormal result triage and predictive outreach for high-risk patients. The achievement of early successes helps doctors trust the technology while creating evidence for future expansion.
Integrate into Clinical Workflow
The implementation of AI tools requires them to integrate naturally with current clinical operations. Systems that fail to integrate properly create more clicks and user frustration while potentially decreasing safety levels. The process of co-design with frontline clinicians leads to the creation of tools which enhance clinical reasoning instead of forcing rigid processes.
Training and Change Management
The training program should teach staff members about AI’s impact on their daily work and how to understand system recommendations and handle situations that require escalation. The system requires defined governance structures to establish roles for model performance accountability and model update responsibilities and incident response management. The system receives continuous feedback which enables real-world use to guide its improvement process.
Measure Outcomes and Monitor for Harm
Success should be tracked with measures like diagnostic accuracy, time on paperwork, patient happiness, and health results. Ongoing checks help catch errors or unfair effects. Strong data rules and system links are vital, with standard formats, access limits, and audit trails. EHR links should use open standards to keep data safe and easy to share. Patients and staff need early talks on privacy and AI’s role, with clear consent, simple explanations, opt-outs, and feedback channels. Payment codes, pilot funds, and grants can ease costs and reward safe use, while rules for data sharing, privacy, and training ensure AI boosts care fairly and avoids uneven results.
Real-World Examples and Case Scenarios
The following examples demonstrate how AI transforms daily operations in primary care settings. The cases demonstrate both basic preventive care outreach and sophisticated diagnostic assistance for unclear medical presentations.
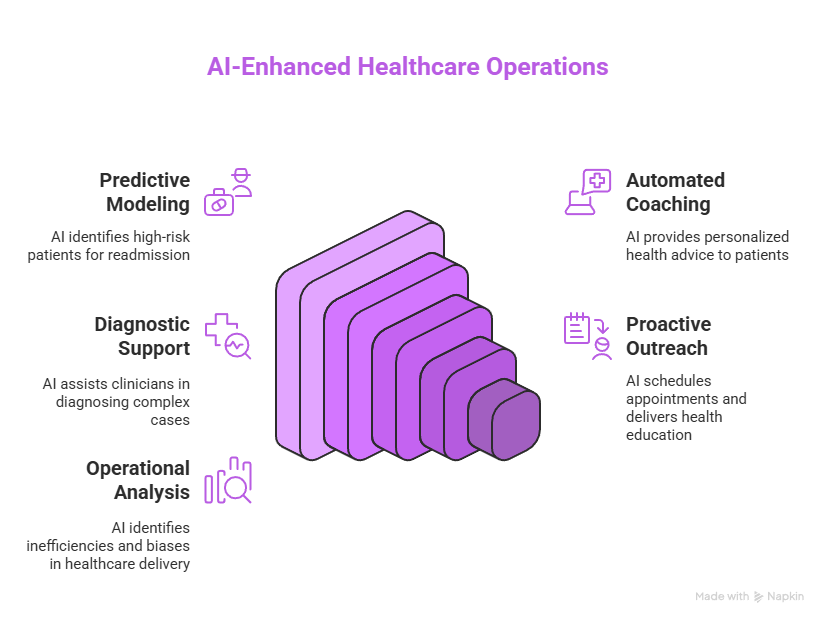
Scenario: Reducing Hospital Readmissions
A clinic implements predictive modeling to detect patients who face elevated readmission risks during the first thirty days after hospital discharge. The system generates automated lists which care managers use to contact high-risk patients for medication reconciliation services and home health referrals and early follow-up appointments. The program leads to decreased preventable readmissions while enhancing care continuity and reducing total healthcare expenses.
Scenario: Improving Diabetes Control
Remote glucose monitoring devices transmit data to an AI platform which analyzes behavioral patterns that lead to hyperglycemia. The system sends automated coaching messages to patients but sends flagged patients to clinicians for asynchronous review. The panel experiences a decrease in hemoglobin A1c levels while urgent hyperglycemic events become less frequent.
Scenario: Enhancing Diagnostic Safety
The AI decision support system prompts the clinician about possible differential diagnoses when specific symptom clusters appear during patient visits. The system detects an unusual pulmonary embolism case which results in immediate imaging and treatment procedures that would have been delayed otherwise.
The practical application of AI models involves proactive preventive care outreach through analysis of claims data and lab results and visit histories to identify patients who need cancer screenings and immunizations and chronic disease maintenance visits. The system uses automated text or portal messages to schedule appointments and deliver targeted education while care teams handle patients who need individualized navigation. The clinics achieve better screening results and earlier cancer diagnoses of colorectal and cervical cancer through workflows that transfer routine reminder duties from clinical staff.
Multiple healthcare organizations have started using AI systems to identify operational delays and unequal service distribution. The analysis of visit notes through natural language processing together with triage pattern analysis helps identify patient groups who receive insufficient preventive counseling and experience prolonged wait times which leads to quality improvement initiatives. The combination of algorithmic predictions with clinician-led audits enabled the detection of referral pattern bias while maintaining clinical relevance of alerts which preserved trust and enhanced safety and access.
Limitations and Ongoing Challenges
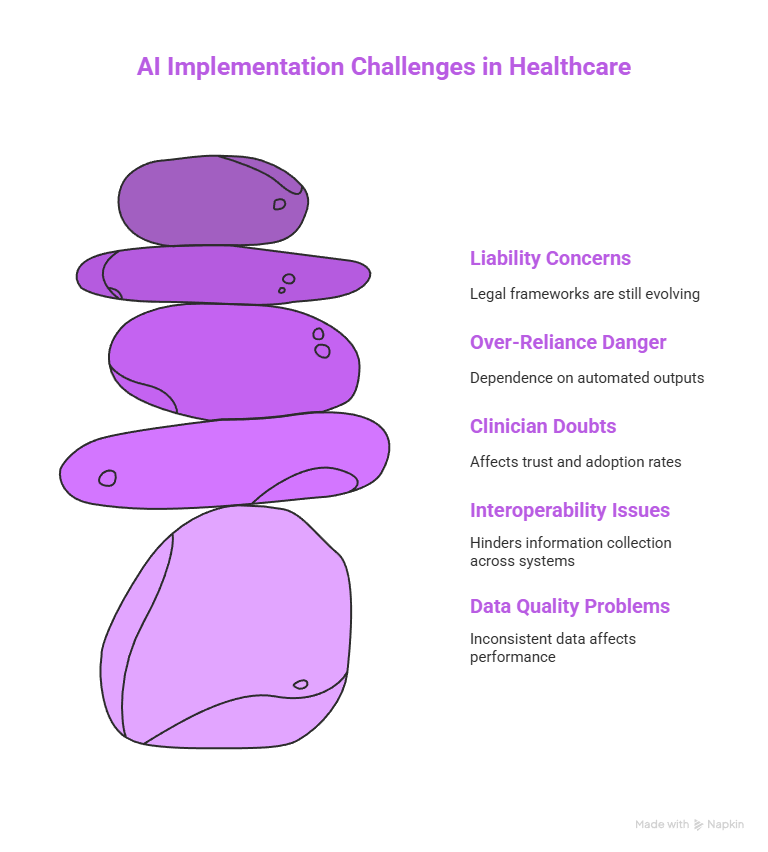
AI is not a panacea. The system faces multiple challenges including data quality problems and interoperability issues and clinician doubts and the danger of depending too heavily on automated outputs. The solution to these challenges demands financial support for data infrastructure development and governance systems and ongoing clinician education programs.
Data Quality and Interoperability
The primary care clinics operate with different EHR systems and maintain inconsistent levels of data completeness. The performance of AI systems requires both high-quality structured data and the capability to collect information from different care environments. The reliable application of AI-driven insights depends on strong interoperability standards together with robust data pipelines.
Human Factors and Trust
Trust is essential for clinician acceptance. The combination of model performance transparency with visible safety measures and clinician override capabilities helps build trust among healthcare providers. The presentation of actionable concise information through interface design reduces cognitive load which leads to better adoption rates.
Liability and Responsibility
The development of legal frameworks for AI-enabled decision liability continues to progress. The tools must enable clinicians to document their reasoning clearly because they maintain full responsibility for their care decisions. Professional societies together with insurers and regulators work to establish clear expectations about how AI should function in clinical practice.
Looking Ahead: Practical Predictions for the Next Five Years
AI will reach its peak of development in the near future when data remain consistent and tasks have clear definitions. The standardization of documentation automation and inbox triage and risk stratification capabilities will occur in numerous primary care facilities. Patient-facing tools will grow through the implementation of hybrid systems which unite automated guidance with clinical supervision.
Greater Emphasis on Federated and Privacy-Preserving Learning
The use of federated learning techniques will increase because they enable institutions to train models together without revealing patient data thus protecting privacy. The method enhances model generalizability and decreases deployment biases.
Stronger Focus on Equity and Real-World Validation
The combination of regulatory requirements and payment system demands will force vendors to show their products work effectively in real-world settings with different patient groups. The development and deployment of products will require mandatory equity audits together with bias mitigation strategies and community involvement in design processes.
Integration with Primary Care Teams
AI will function as a part of clinician workflows and team roles. AI-powered task lists together with triage scores and patient education materials will serve as essential tools for nurses and medical assistants and community health workers to provide proactive team-based care.
Practical Checklist for Clinics Considering AI
The process of preparing primary care practices for AI adoption requires both clinical and technical and organizational steps. The checklist contains essential considerations for safe and effective implementation.
Pre-Implementation
The first step is to identify particular challenges where AI solutions can deliver quantifiable improvements. Stakeholder engagement: Involve clinicians, IT staff, administrators, and patients in selection and design. Data readiness: Assess data quality, completeness, and interoperability.
Implementation
The implementation process should start with controlled workflow integration to minimize disruptions during the transition. Training: Provide role-based training and establish escalation pathways. Governance: Create accountability structures for monitoring performance and addressing incidents.
Post-Implementation
The monitoring process should track clinical outcomes together with safety events and user satisfaction and equity metrics. Iteration: Update models and processes based on real-world feedback. Communication: Keep patients informed about AI use and data practices.
Trending Now!
The health system depends on primary care but this essential component operates at financial deficits while dealing with insufficient physicians and expensive operations and excessive patient responsibilities. Patients who maintain regular access to primary care services experience superior health results despite facing various challenges. AI technology enables PCPs to enhance their operational efficiency through evidence-based resource matching and patient context understanding and workflow optimization. The AI tool TOM from Lumeris together with UpToDate® demonstrates how technology functions as an additional care team member which provides immediate patient-specific recommendations directly to healthcare professionals during their workflow.
The AI system supports patient care through three functions which include preparing summaries and triaging needs and delivering personalized educational content based on language skills and literacy level and medical diagnosis. The system decreases missed questions while enhancing patient participation and enables staff to focus on treating complex medical cases. The integration of EHR systems enables AI to present both clinical and educational content at appropriate times which benefits healthcare providers and their patients. The combination of evidence-based content with AI delivery systems will transform primary care into a more effective sustainable patient-centered healthcare system.
Conclusion: Balancing Innovation with Care
AI technology has the potential to transform primary care through its ability to enhance precision while delivering personalized care and better patient satisfaction and reducing administrative tasks. The implementation of these benefits requires strategic deployment alongside strict monitoring and dedication to maintaining fairness and privacy standards. AI systems function best when used alongside clinicians and patients to enhance human care elements such as listening and empathy and healing instead of replacing them.
The path to real change begins with addressing specific clinical requirements through real-world testing while maintaining transparency and fairness. The correct implementation of AI technology will transform primary care into a faster and smarter system that remains human-centered for every patient.
The AI solutions at Helpsquad Health enable practices to access proven benefits through safe implementations. Begin your free trial today or join us now to discover how our solutions can enhance care delivery while reducing delays and establishing enduring patient trust.


