Ambient AI Scribes and Documentation Automation: A Doctor’s New Best Friend
02 Sep 2025 By: Maria Rush
Updated
Clinical documentation is one of those things that’s necessary but no one really enjoys it. After a full day of seeing patients, the last thing most doctors want to do is sit down and type notes into an EHR. And yet, that’s exactly what’s been happening for years. But now we’ve got something different: ambient AI scribe.
These are like quiet digital assistants that listen in on doctor-patient conversations and magically (okay, not magically, but close) draft up clinical notes in the background. Yep, no more typing while trying to maintain eye contact.

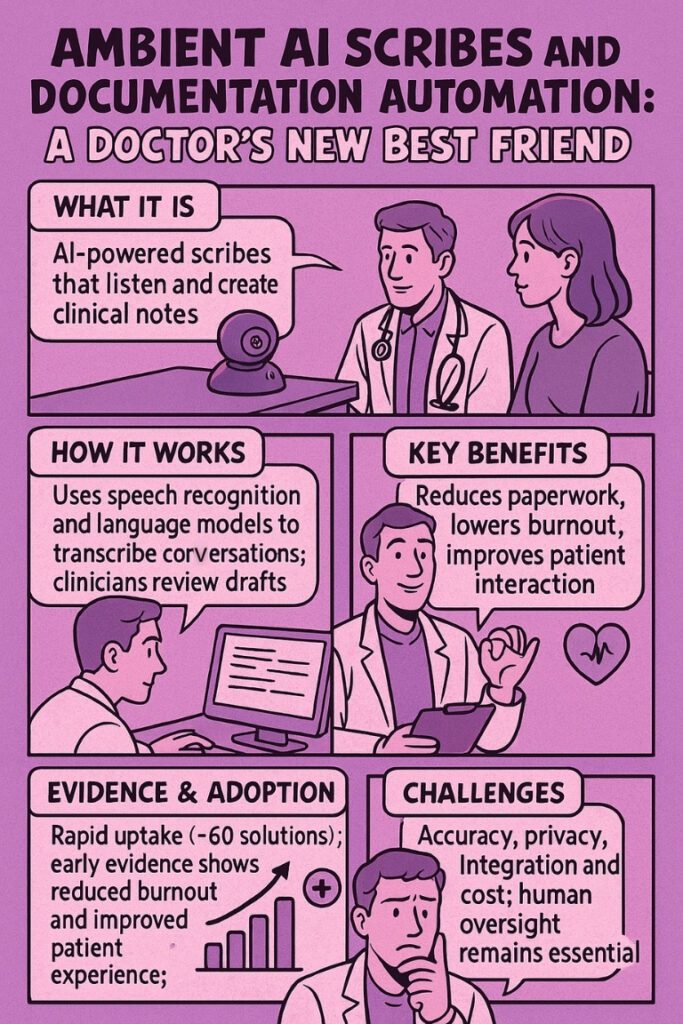
What is Ambient AI Scribe?
Ambient AI scribe, also called digital scribes, use speech recognition and large language models to “listen” during appointments. They’re not interruptive like traditional dictation tools. Instead, they blend into the background, pick up the conversation, and start forming a clinical note.
They evolved from transcription tools but took a big leap forward when AI started understanding context and nuance. The best part? They try to match the clinician’s writing style. Like having a mini-you taking notes.
How Do They Work? Pretty Seamlessly.
Here’s a quick peek behind the curtain:
- Start the Visit: The doc taps a button in the EHR. The system kicks in and connects to the patient chart.
- Listen and Draft: As the visit unfolds, the system listens, picks up relevant clinical data (like symptoms and exam results), and builds a draft note.
- Review and Sign: The doctor reviews the note, edits as needed, and signs off. Bonus: it can auto-populate structured fields and billing codes.
Why Ambient AI Scribe Actually Matters
Look, everyone talks about “burnout,” but this is a real solution. According to the 2025 PHTI report, ambient scribes can:
- Cut down on after-hours charting
- Help doctors be more present with patients
- Reduce stress (a lot!)
Doctors say it best: “I finally looked my patient in the eye again.”

Evidence and Adoption of Ambient AI Scribe
According to PHTI, around 60 ambient AI scribe solutions were already in play by 2025. That’s lightning-fast adoption for healthcare tech, which usually takes forever to spread.
- Some hospitals reported up to 40% less burnout in doctors using these tools.
- Patient satisfaction also improved because when the doc isn’t glued to a screen, you feel heard.
That said, not everyone saves time. Some doctors with already-optimized workflows didn’t see much difference. And some only use scribes for certain types of visits.
Real-World Examples
UCSF Health gave ambient scribes a shot in 2023 with 100 doctors. The results?
- Drafts were fast.
- Docs still needed to edit.
- But engagement improved, and stress went down.
And studies published in JMIR Medical Informatics showed that ambient scribes:
- Reduced after-hours EHR work
- Improved patient interaction
- But still required careful oversight to avoid errors or weird note formatting
TRENDING NOW
The Permanente Medical Group gave AI scribes a real shot, and wow, did it pay off. After just one year and over 2.5 million visits, doctors saved more than 15,000 hours of typing. That’s like 1,800 full days of paperwork gone. What did they get back? Time with patients. Less burnout. Better conversations. And the patients noticed it too less screen-staring, more actual eye contact. Even after switching vendors mid-way, doctors kept using the tool like nothing happened. It’s not perfect, but it’s proof that when you implement AI the right way, it doesn’t replace people but helps them show up better.
Challenges of Ambient AI Scribe
No technology is perfect. Here’s what to watch out for:
- Accuracy: Drafts might include errors or leave things out. Some even hallucinate (yep, that’s a thing).
- Consistency & Style: Not all notes sound like the doctor wrote them. Editing is still needed.
- Privacy: Since these systems record full conversations, HIPAA compliance is critical.
- Cost: Prices vary, and not everyone’s convinced the ROI is there yet.
- Adoption: Clinicians still need training. Integration with EHRs can be a headache.
Quick Summary
| Aspect | Summary |
|---|---|
| What it is | AI-powered assistant that listens and writes notes |
| How it works | Uses speech recognition and language models to transcribe conversations; docs edit and sign |
| Benefits | Reduces admin work, lowers burnout, helps patient connection |
| Adoption | 60+ solutions by 2025, rapid uptake, mixed time-savings |
| Challenges | Accuracy, privacy, cost, integration. You still need humans |
Conclusion
If you are someone who has spent far too many nights catching up on charting, I find the promise of ambient AI scribes compelling. These tools listen quietly, draft notes almost instantly and will help you focus on the human being in front of you. Early evidence points to meaningful reductions in burnout and better patient interactions.
But this isn’t a panacea. We still need to review and edit the drafts, protect privacy and weigh the costs and benefits. With careful implementation and ongoing research, ambient scribes could make medical documentation more humane and efficient. For now, they’re a promising partner, not a replacement.
Need help bringing AI efficiency to your practice without losing the human touch?
HelpSquad’s HIPAA-compliant virtual assistants and live chat agents work alongside your team. They help reduce admin burden, improve patient communication, and keep documentation workflows running smoothly.
Talk to us and see how we can support your healthcare operations today.