How to Schedule Patients Effectively: A Comprehensive Guide
06 Aug 2025 By: Mary Dellosa
Updated
Efficient scheduling drives strong healthcare delivery. It boosts resource use, cuts wait times, lifts care quality, and improves patient satisfaction.
This guide shares key strategies and tools to help clinics and hospitals on how to schedule patients effectively and book smarter. Better scheduling means better results for both staff and patients.
Understanding the Importance of Effective Patient Scheduling
What is the The Impact on Patient Experience?
Patient satisfaction links to their full visit experience. Scheduling is often the first step. A 2023 MGMA study found that 6 out of 10 patients picked their doctor based on how easy it was to book an appointment.
Improve patient scheduling efficiency makes life easier for patients. Patients can book in minutes, get gentle reminders, and avoid long waits. Easy-to-use apps let them choose times and even meet doctors from home. It feels personal.
Operational Efficiency and Financial Health
Poor scheduling can leave staff idle, pack waiting rooms, and strain admin teams. NIH says missed visits cost U.S. healthcare about $150 billion each year. Better scheduling cuts no-shows, boosts provider output, and supports steady income. It also spreads work fairly, easing stress and lifting team morale.
Tools like smart algorithms and data help clinics plan ahead. They can match staff to demand and improve care. Telehealth adds flexibility to meet more needs.
How to Schedule Patients Effectively: Key Strategies for Success?
1. Prioritize Patient-Centered Scheduling
Patient-centered scheduling puts patient needs first. It offers flexible times, urgent slots, and easy booking by phone, app, or online.
It also respects patient diversity. Language help and longer hours can make care easier to reach. Feedback from surveys helps improve the system over time.
2. Implement Time Slot Optimization
Not all visits take the same time. A quick check-up needs less time than a full exam. Good scheduling gives each visit the time it needs. A quick refill might take 15 minutes, while a first visit could need 45. Short breaks help avoid running behind.
3. Use Data-Driven Scheduling
Look at patterns to see when patients cancel or don’t show up. If Mondays are slow, send reminders or slightly overbook to keep things moving.
Paying attention to patient habits makes scheduling feel personal. Simple texts or emails can remind them and help them stick to their care plan.
What are the Strategies to Reduce No-Shows and Cancellations?
Automated Appointment Reminders
A quick, kind reminder a day or two before says, “We’re here for you.” It helps patients remember and gives them time to change plans if needed. Using their name and visit info makes it feel personal. A warm message like, “Hi [Name], we look forward to seeing you,” builds trust and shows you care.
Flexible Rescheduling Options
Life happens, and plans change. When rescheduling is easy, by phone or online, patients feel more comfortable reaching out instead of just missing the visit. Clear messages that explain why it helps to reschedule early build trust. It shows respect for their time and yours, and keeps things running smoothly.
Implementing Waitlists and Overbooking Carefully
Waitlists help fill spots when others cancel, so no time goes to waste. Careful overbooking can also help, but only if it doesn’t stress staff or patients.
Let patients mark how urgent their need is. This helps give faster care to those who need it most. Clear updates keep patients informed and reduce stress.
Leveraging Technology for Smarter Scheduling
Electronic Health Records (EHR) Integration
Modern EHRs link scheduling with patient records and billing. This keeps things smooth, cuts errors, and helps teams plan visits the right way.
With quick access to a patient’s history, staff can book the right time. If someone has ongoing issues, they get the time they need to be heard and cared for.
Online Patient Portals and Mobile Apps
Online portals and apps let patients book or change visits anytime. This ease lifts stress off staff and keeps patients more involved in their care. These tools offer waitlists, doctor choices, and telehealth visits. Reminders help cut no-shows. Patients can also learn more about their health in one place.
Artificial Intelligence and Predictive Analytics
AI tools now help predict no-shows, set smart visit times, and suggest best slots. They learn from past data to keep schedules smooth and patients happy. AI also helps plan staff and gear needs, cutting delays. As it grows, it will change how clinics book visits and care for people—faster and more personal.
Best Practices for Staff Training and Workflow Design
Training Front Desk and Scheduling Staff
The team handling appointments plays a big role in patient care. They need to listen well, use the tools easily, and treat each patient with care and respect.
Training helps staff meet people where they are, some like a quick text, others feel better hearing a friendly voice. With practice and support, they gain trust and grow.
Designing Efficient Scheduling Workflows
Set clear steps for booking, confirming, and following up. Use simple templates and keep staff and care teams in sync to avoid mistakes and patient stress.
A central system helps everyone stay updated. A friendly text or email reminder helps patients feel remembered, stay on schedule, and know their health truly matters to you. Listening to staff and patient feedback keeps the process smooth and human.
Handling Special Cases in Scheduling
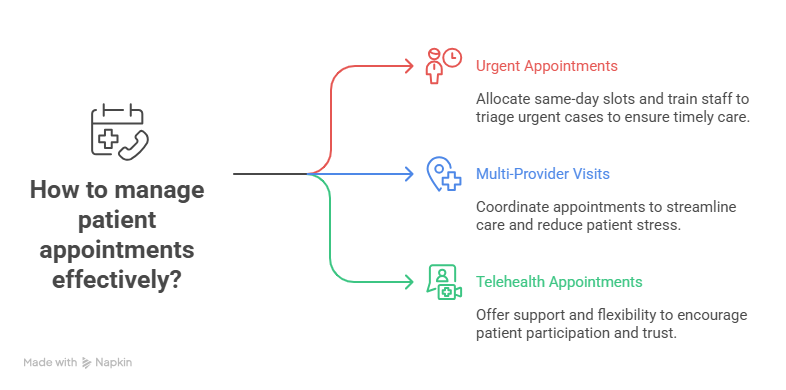
Managing Urgent and Emergency Appointments
Routine visits can be booked early, but urgent needs need wiggle room. Save time slots for same-day or walk-in care to help patients get seen fast. Teach staff how to spot urgent cases and use clear triage steps. Real-time updates on openings keep wait times low and help patients feel cared for.
Coordinating Multi-Provider Visits
Patients with complex needs often see many doctors. Booking their visits together saves time and stress, making care feel more connected.
When care teams use one system, nothing gets missed. A care coordinator acts like a guide, making sure the patient feels heard, helped, and never alone.
Accommodating Telehealth Appointments
Some patients feel nervous about video visits. A kind voice, simple steps, and patience can help them feel safe and ready. Letting them choose what feels best online or in person shows you care. When patients feel seen and supported, they show up and trust you more.
Outsourcing Scheduling Services
What are the Benefits of Outsourcing?
Outsourcing scheduling can free up staff and help clinics focus on care. Expert partners bring smart tools and handle booking without big upfront costs.
These services adjust with your needs, using top tech to stay flexible. They also ease staff shortages by keeping things running, even when it’s busy.
Choosing the Right Partner
When outsourcing, pick a partner with strong healthcare experience. They should handle booking, reminders, and offer helpful data tools. Make sure they follow privacy rules and keep patient info safe. They should work well with your current systems and make the switch easy. The right partner can boost scheduling, ease staff load, and make patients happier.
Measuring and Improving Scheduling Performance
Key Performance Indicators (KPIs) to Track
To improve scheduling, keep an eye on key numbers like:
- No-show and cancellation rates
- Patient wait times
- How busy providers are
- Patient feedback on scheduling
- Time between booking and the visit
These numbers tell the real story. Lots of no-shows? Maybe reminders need a boost. Long waits? It could be a timing or staffing issue. Watching these signs helps clinics spot problems early, care better, and make visits smoother for everyone.
Soliciting Patient Feedback
Patients know what works for them. A quick survey or kind ask can show what feels easy and what needs fixing. When you listen, they feel valued. A short chat can build trust and help make care more personal and kind.
Continuous Process Improvement
Scheduling isn’t just set once and forgotten; it changes and grows. Use feedback, data, and staff input to move the process forward, making it work for everyone well. Train your team often, update tools, and stay open to change. When you adapt quickly, you serve patients better and keep care running smoothly.
Trending Now
Physician burnout is a growing issue marked by exhaustion, depersonalization, and low achievement. It stems from long hours, heavy workloads, lack of control, and administrative demands. Personal traits like perfectionism, poor coping, and weak support systems increase the risk. Burnout leads to more medical errors, poor patient care, mental health issues, and higher suicide rates. It also raises healthcare costs through turnover and reduced productivity. Addressing it needs system-level changes, leadership support, flexible work options, and mental health care access.
Conclusion
Good scheduling takes the right mix of people, tools, and care. It means putting patients first, using data smartly, and making booking simple and smooth.
When clinics get scheduling right, care improves, patients stay loyal, and teams work better. As healthcare changes, scheduling must grow with it—always patient-first. Need help improving your scheduling process? HelpSquad health’s services make it easy for patients to book, reschedule, or ask questions anytime.
Why is effective patient scheduling crucial in healthcare?
Effective patient scheduling improves both care and clinic efficiency. It shapes patients’ first impression, reduces wait times, and helps providers use their time better. When scheduling runs smoothly, patients can book easily, wait less, and feel valued, boosting satisfaction and loyalty. For clinics, optimized schedules cut idle time, reduce no-shows, increase productivity, support steadier revenue, and ease staff stress.
In what ways does scheduling impact the patient experience?
For most patients, the experience starts well before the exam room. When scheduling is fast, flexible, and easy, by phone, online portal, or app. Patients feel supported instead of frustrated. Friendly reminders reduce anxiety and show they’re valued. Clear communication, reasonable wait times, and simple rescheduling demonstrate respect for their time and needs. Together, these touches help patients feel like people, not time slots, boosting engagement and encouraging them to return.
What do you mean by patient-centered scheduling, and how does it work in practice?
Patient-centered scheduling is an approach that prioritizes patients’ needs, preferences, and lifestyles over rigid internal routines. It may include offering early, evening, or weekend appointments, keeping slots for same-day or urgent visits, and providing multiple ways to book. It also considers language, mobility, and access to technology, while actively gathering and acting on feedback about scheduling and wait times. The goal isn’t to accommodate everything, it’s to align scheduling options with how patients actually live, work, and seek care.
What ways do clinics find favorable from scheduling time-slot optimization?
Time-slot optimization recognizes that not all visits take the same time or complexity. Instead of using one standard block, you assign shorter slots for quick follow-ups or refills and longer ones for new patients, complex cases, or multiple concerns, sometimes based on patient history. You can also build in buffer periods to absorb overruns and prevent delays from cascading. Reviewing actual time spent by visit type helps set more accurate slot lengths, reducing waiting and bottlenecks while creating a smoother day for both patients and providers.
How to significantly reduce no-shows and last minute cancellations?
Reducing no-shows takes a mix of respect, flexibility, and smart reminders. Use automated texts, emails, or calls at well-timed intervals so patients remember without feeling nagged. Make rescheduling simple so they’re more likely to cancel or change early instead of not showing up. When cancellations happen, use a waitlist to fill open slots quickly. Some clinics also use limited overbooking in time blocks with historically high no-show rates. Most importantly, explain why timely cancellations matter, so another patient can be seen sooner, so patients feel involved rather than penalized.