How to Use Telehealth for Better Patient Care
22 Sep 2025 By: Mary Dellosa
Updated

Telehealth has changed how care is given, opening new ways to treat patients. Tech growth and COVID-19 made it key in today’s medicine, not just a trend. This article shows how to use telehealth to boost care, reach more people, and cut delays in treatment.
Understanding How to Use Telehealth: Beyond Virtual Visits
Telehealth offers more than video calls. It covers remote monitoring, mobile apps, messaging, email, and teletherapy. Using all these tools boosts care and keeps patients more involved. This helps doctors treat issues early, leading to better results and happier patients.
In 2023, the American Medical Association found over 80% of doctors were using telehealth. But telehealth isn’t just a backup. When used every day, it helps people stay healthy, saves money, and brings care to those who live far from a doctor.
Types of Telehealth Services
There are three primary categories of telehealth services:
- Live Video Conferencing: Real-time interactions between patients and providers, ideal for consultations, follow-ups, and mental health services.
- Remote Patient Monitoring: You use simple devices at home to track things like blood pressure or sugar levels. Your doctor checks the data to keep an eye on your health.
- Store-and-Forward: You send images, test results, or health info to your doctor. They review it later and get back to you with advice or next steps.
Each kind of telehealth helps in a simple, helpful way. Video visits are great if you can’t travel or live far from a clinic. Remote tools let your doctor watch things like blood pressure or sugar levels and check in if something seems off. With store-and-forward, you can send photos or test results, and your doctor looks at them later. You still get expert care without needing to go in right away.
Telehealth is more than quick visits. It helps people stay healthy and manage ongoing issues. Apps let patients check progress, remember pills, and learn what they need. This brings patients and doctors closer, builds trust, and makes care easier to follow for better health.
Enhancing Access to Care Through Telehealth
A big benefit of telehealth is how it removes distance and travel limits. People in rural areas, with mobility issues, or busy lives can reach care more easily. It makes getting advice simpler and builds a more open system where patients feel free to get help without time or place holding them back.
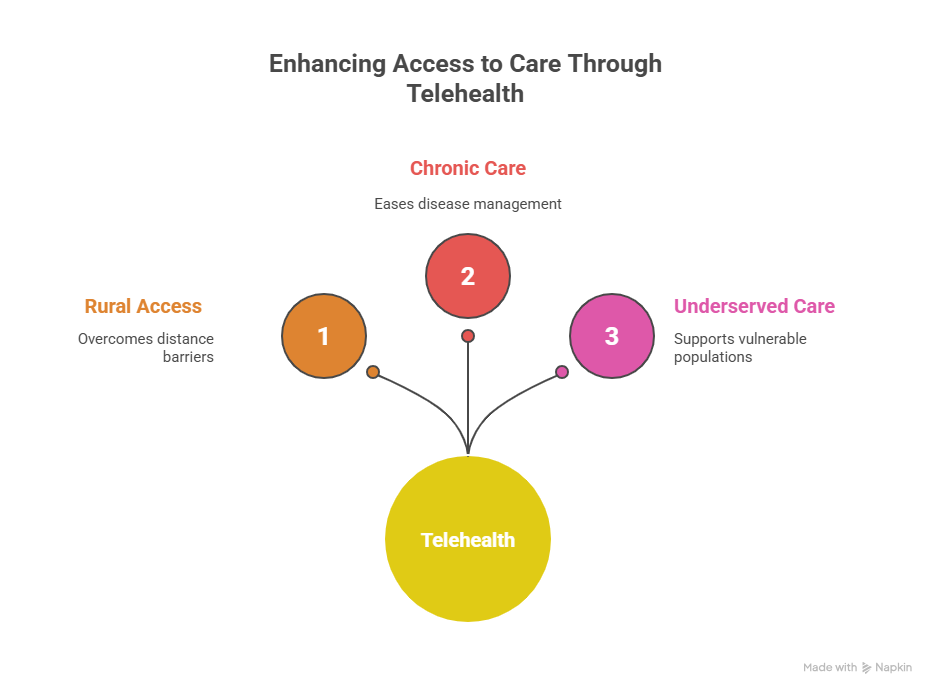
Addressing Rural Healthcare Disparities
Many rural towns don’t have enough doctors, and patients often drive hours for care. Telehealth helps by letting them meet with doctors and specialists online. The Veterans Health Administration uses it to give veterans in remote areas mental health support, improving follow-up and lowering hospital stays. It also trains local providers, keeping them updated and able to give strong care in their towns.
Supporting Chronic Disease Management
Living with diabetes, high blood pressure, or heart disease can feel overwhelming. Telehealth eases the load by tracking health daily and letting doctors step in sooner. One study showed heart patients using remote monitors went back to the hospital far less often. Telehealth also gives simple guides and custom care plans, helping people stay involved and feel more in control of their health.
Improving Care for Underserved Populations
Telehealth helps underserved groups like low-income families and people with disabilities. It removes travel stress and offers flexible visits, making care easier to keep. Many platforms are simple to use, so people with any tech skill can join. Training programs give extra support, helping patients feel included and connected while getting the care they need.
Best Practices for Implementing Telehealth in Clinical Settings
Bringing telehealth into care takes careful planning and clear steps. This part shares key tips for providers who want to make the most impact for patients.
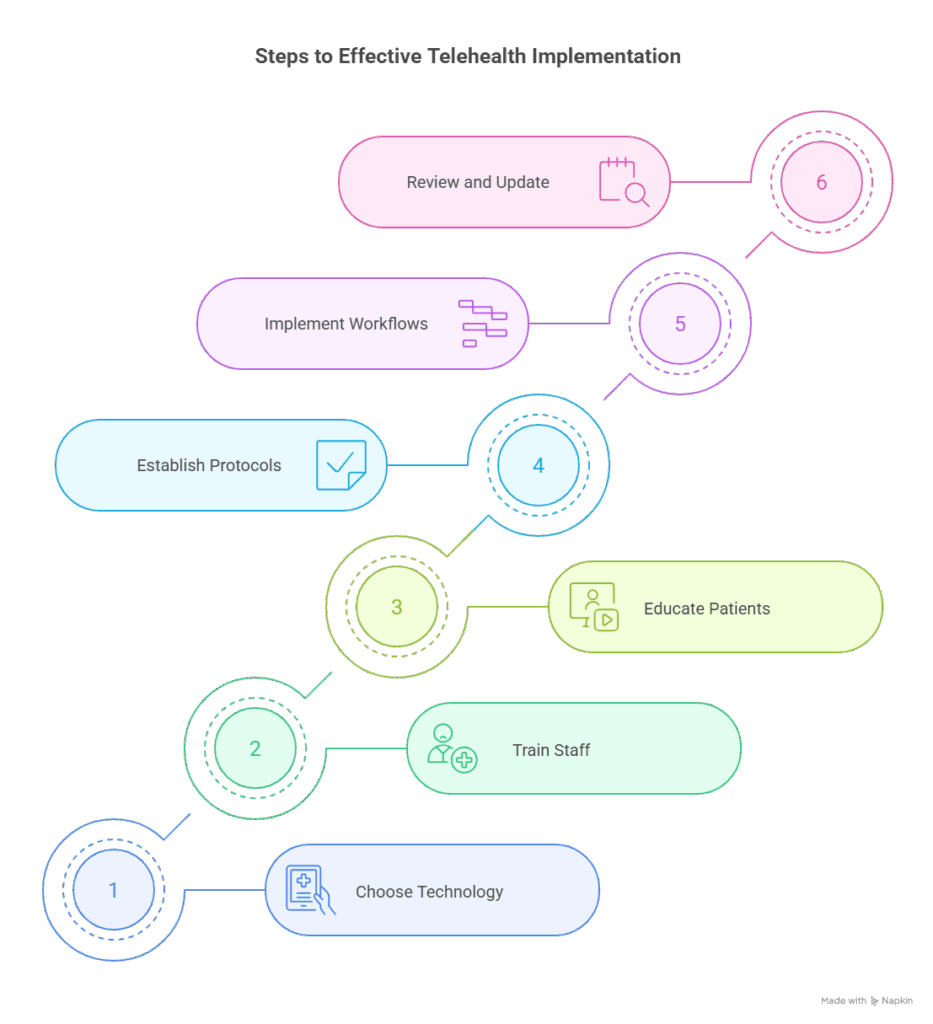
Choosing the Right Technology
The right telehealth platform makes care smoother. It should be simple, safe, and work on any device. It must also follow HIPAA rules to protect patient privacy. Linking it with EHR systems helps records stay clear and care stay connected. Helpful tools include video visits, live chat, and remote monitoring. Providers should test options, gather staff and patient feedback, and pick the system that fits their needs best.
Training Staff and Educating Patients
Both doctors and patients need practice to feel at ease with telehealth. Doctors should build clear online communication, learn simple tech fixes, and know when a visit needs to be in person. Role-play can build skill and comfort. Patients need simple steps for visits, device use, and privacy rules. Guides like videos or FAQs can boost confidence and make care smoother, leading to better results.
Establishing Clear Protocols and Workflows
Defining when telehealth is appropriate versus in-person visits is crucial. Providers should develop clinical protocols that outline patient selection criteria, documentation standards, and follow-up procedures. Strong scheduling and telehealth coordinators help cut no-shows and keep care moving. Providers should update rules often using new practices and patient feedback. This steady review builds a flexible system that keeps improving for both patients and doctors.
Improving Patient Engagement and Satisfaction Through Telehealth
Being involved in care can shape health. Telehealth helps patients feel closer to doctors and more in charge. With new tools, care feels faster, easier, and built around the patient.
Enhancing Communication and Convenience
Telehealth makes it easier for patients to connect with doctors without travel or long waits. This ease often leaves patients happier. Flexible hours also cut stress for people juggling work and family. This freedom helps patients stay involved and take charge of their care.
Personalizing Care with Remote Monitoring
Remote health tools give people instant updates, making daily care easier. Someone with diabetes can see sugar levels right away and choose what’s best in the moment. Many devices link to simple apps that track progress, send pill reminders, and share info with doctors. This keeps care personal, gives patients confidence, and helps doctors give the support that truly fits.
Addressing Barriers to Telehealth Adoption
Not everyone finds telehealth easy. Some may struggle with tech, language, or no internet. Doctors can help with simple tools, phone visits, and support in many languages. Local groups can teach patients, give devices, or offer Wi-Fi. By removing these hurdles, more people especially those in need can get the care they deserve.
Legal, Ethical, and Reimbursement Considerations
To keep telehealth strong, providers must follow rules. They need to handle licenses, patient consent, and payment policies to give safe and fair care.
Licensing and Cross-State Practice
Treating patients across state lines can make telehealth tricky. Some states joined licensure compacts to make it easier, but rules still vary. Doctors must check state laws on records, follow-ups, and which services can be done online. Since laws keep changing, providers need to stay updated and speak up for better rules.
Informed Consent and Privacy
In telehealth, patients should give clear consent after learning the pros and cons. Care must stay private with safe platforms. Patients can also help by joining visits from a quiet space and sharing info carefully. These steps build trust and make online care feel safe and personal.
Reimbursement Policies and Billing
Today, more insurers, including Medicare and Medicaid, pay for telehealth visits. But rules still differ, so providers must stay updated to avoid denied claims. Keeping clear notes and talking openly with patients about possible costs helps build trust. Billing experts can also guide the process, freeing doctors to focus on care. Understanding these money details is key to keeping telehealth available for the future.
Future Trends and Innovations in Telehealth
Telehealth is growing fast with new tech and rising patient needs. By staying updated on trends, providers can spot fresh ways to improve care.
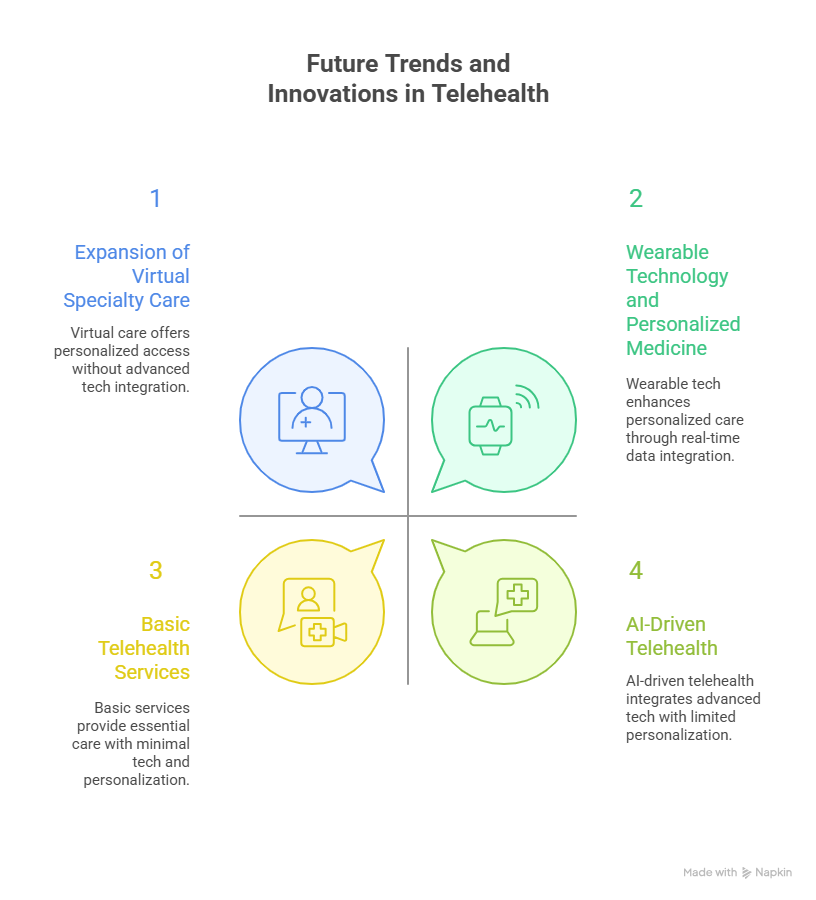
Integration of Artificial Intelligence and Machine Learning
AI is making telehealth more caring and simple. It can spot early health issues and alert doctors quickly. It also handles paperwork, giving doctors more time with patients. Soon, AI may act like a helpful guide, answering questions and sharing easy, personal health tips.
Expansion of Virtual Specialty Care
Specialists like dermatologists, psychiatry, and cardiology now meet patients online. This saves travel and makes checkups or second opinions easier. Doctors can also team up through telehealth, giving patients more complete care. Sharing records quickly means fewer repeat tests and faster decisions for better health.
Wearable Technology and Personalized Medicine
New wearable devices track more than heart rate, they follow sleep, activity, and even stress. This info helps create care plans that fit each person better. When linked to telehealth, doctors can see updates in real time and step in early if needed. Smarter data tools also reveal patterns doctors might miss, leading to stronger, more personal care. This gives patients more control and confidence in their health journey.
Trending Now
A Stanford Medicine–led study published in Mayo Clinical Proceedings found that while U.S. physician burnout rates declined in late 2023 and early 2024 compared to pandemic highs, they remain alarmingly elevated, with 45.2% of doctors reporting at least one symptom of burnout. Women physicians and those in high-demand specialties like emergency and internal medicine are disproportionately affected. Although improved from 62.8% in 2021, doctors are still 82.3% more likely to experience burnout than other U.S. workers, fueling risks of turnover, reduced clinical hours, and worsening patient care. Experts warn that with a projected shortage of 86,000 physicians by 2036, addressing administrative burdens, regulatory strain, and work-life imbalance has become a national priority for sustaining the medical workforce and safeguarding healthcare quality.
Conclusion: Embracing Telehealth for a Healthier Future
Telehealth makes it easier for people to see a doctor, stay involved in their care, and catch problems early. With the right tools, care feels simple and personal. As healthcare changes, telehealth will keep helping people get fair and easy access to the care they need.
Helpsquad Health’s virtual assistant services make telehealth even smoother. Their live chat and support team guide patients through scheduling, tech setup, and questions before visits. This extra help reduces stress, saves time, and keeps patients more engaged in their care. By handling these details, Helpsquad Health lets doctors focus on what matters most, supporting their patients.


