Predictive Analytics in Denial Management
05 Aug 2025 By: Maria Rush
Updated
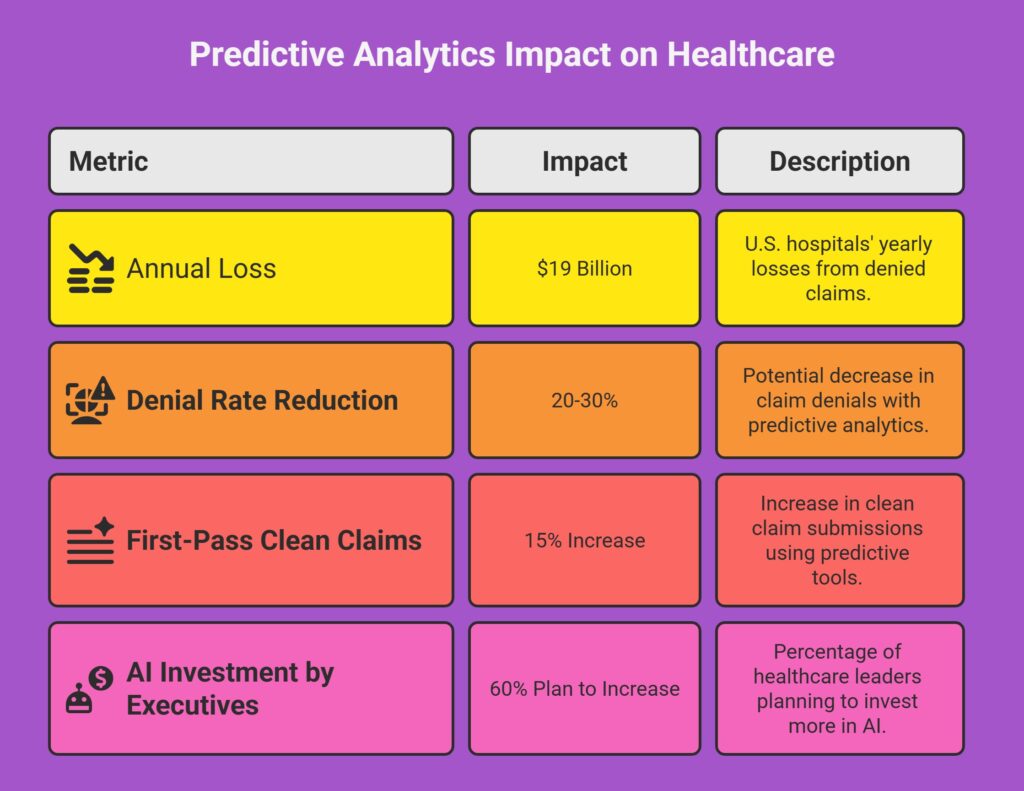
Managing revenue in healthcare is like trying to plug holes in a leaky bucket. Just when you think everything’s under control, a denied claim slips through and throws everything off. Denials have always been part of the process, but now they’re piling up fast. Hospitals reportedly spend around $19 billion a year just trying to reverse them.
You don’t have to wait for those denials to land. Predictive analytics lets you get ahead of the mess. It’s like looking at the radar before a storm, you can spot problems before they actually hit.
This guide takes a look at how predictive analytics is helping providers take a more proactive approach to denial management, what the real benefits are, and how to start using it without getting overwhelmed.

What is the Challenge of Denial Management in Healthcare?
The Scope and Impact of Claim Denials
Claim denials are one of those things that chip away at revenue slowly but steadily. The average denial rate is about 5–10%, but depending on your specialty, it might be even higher. And when you’re talking about thousands or millions of claims, even a small percentage can make a big dent in revenue.
Denials happen for all sorts of reasons: a missing code, outdated documentation, eligibility mismatches, or rule changes from payers. Chasing down these errors eats up staff time. The AMA says providers spend $15 billion every year dealing with this.
And the fallout isn’t just financial. Slower cash flow can mean fewer resources for patient care. When admin teams are buried in resubmissions, it’s harder to focus on what really matters, patients.
Traditional Denial Management: Reactive and Resource-Intensive
For a long time, predictive denial management system was about reacting. A claim got denied, the team looked into it, and tried again. It’s time-consuming, inefficient, and often frustrating.
This kind of process makes it hard to see trends. Why do denials spike every March? Is it one department, or one payer? Without that insight, it’s like fighting the same fire over and over.
That’s why more healthcare organizations are looking to data-driven tools that show them the problems before they start.
What Is Predictive Analytics and Why It Matters in Denial Management?
What is Predictive Analytics in Healthcare Finance?
Predictive analytics takes what’s happened in the past. Claim history, payer behavior, documentation patterns, and runs it through statistical models and machine learning. The result? You get a good idea of which claims are likely to hit a snag before they’re sent off.
Think of it as having a radar for red flags. Instead of flying blind, you’re given a heads-up when something doesn’t look right.
How Predictive Analytics Enhances Reporting and Decision-Making?
Instead of just reporting what went wrong last quarter, predictive analytics gives you real-time info that helps you act now:
- Shows which claims have the highest risk of getting denied.
- Pinpoints common errors tied to certain procedures or documentation.
- Projects how much revenue could be at risk.
- Suggests what to fix to boost the chances of getting paid the first time.
This kind of visibility makes it easier for billing and clinical teams to stay on the same page and avoid costly repeat mistakes.
Trending Now
Predictive analytics used to be something only big companies or data teams talked about. Now, with AI in the mix, it’s something more people are starting to use because it actually helps. It looks at what’s already happened in your business and shows you what’s likely to happen next. Not as a guess, but as a pattern backed by real data. AI speeds this up by doing the analysis for you, so you’re not stuck looking at spreadsheets and wondering what it all means. You get useful info, fast. Things like: when to expect a drop in demand, which areas might need more attention, or how to adjust before a problem gets bigger. It’s not flashy. But it works. And the more you use it, the easier it gets to make decisions that actually move things forward.
What are the Key Benefits of Predictive Analytics in Denial Management?
1. Reducing Denial Rates Through Proactive Intervention
When predictive tools flag a claim before it’s submitted, teams can fix errors like missing attachments or mismatched codes right away. Some studies say denial rates can drop by 20–30% with these tools.
It’s not just about saving money. It’s also about saving time and giving teams room to focus on more complex cases.
2. Improving Financial Forecasting and Revenue Cycle Efficiency
Predictive models don’t just reduce denials. They help teams prepare for what’s ahead. If denial trends spike during flu season, or when a payer changes policy, the model picks it up early.
That means you can shift staff, adjust timelines, and avoid getting blindsided.
3. Enhancing Collaboration Across Departments
Denials aren’t just a billing issue. Often, it’s a mix of coding, documentation, or payer-specific rules.
Predictive tools give every team access to the same insights. Clinicians see where documentation needs work, coders catch recurring errors, and billing teams can prioritize risky claims.
When everyone’s working with the same data, communication improves, and claims move faster.
Implementing Predictive Analytics for Denial Management: Best Practices
Data Quality and Integration Are Foundational
Predictive analytics only works if the data feeding it is clean, current, and coming from the right sources. That means making sure your claims, documentation, and payer info are all integrated into one system that can talk to itself.
Bad data equals bad predictions, no matter how fancy the model is.
Start with Targeted Use Cases and Pilot Programs
Instead of jumping in with every claim type and payer, pick one area to start with. Maybe it’s a common procedure or a tricky payer.
Start small, prove the results, and build from there.
Leverage Advanced Analytics Tools and Expertise
You don’t have to do this alone. There are companies out there who specialize in analytics for healthcare billing and revenue cycles. They’ve got tools and models ready to go, and many are user-friendly enough that your staff won’t need a data science degree.
Training is very important. Your team needs to know not just how to read the reports but how to act on what they’re seeing.
Continuously Monitor, Refine, and Adapt Models
Things change fast in healthcare. Payer rules, medical codes, and clinical workflows evolve constantly. Your predictive model needs to keep up.
Set up a review process so you can tweak the system as new issues emerge.
Real-World Examples of Predictive Analytics in Denial Management
- Predictive analytics in practice: Some healthcare systems that adopted predictive analytics alongside their EHR platforms reported up to a 25% drop in claim denials within six months, and a 10–15% improvement in clean claim rates.
- Revenue cycle insight: Studies show that RCM firms leveraging analytics to spot payer trends have seen denial reductions of around 10%. Especially when using that data to improve workflows and negotiate clearer policies.
What are the Challenges and Considerations When Adopting Predictive Analytics?
Data Privacy and Security
You are handling confidential information, therefore, security is a priority. This involves total HIPAA compliance, encryption, and strict access controls. In the event that you are collaborating with a third-party vendor, ensure that their standards are equal to or better than yours.
Change Management and Staff Buy-In
Any time you change a system, people push back. The best way to ease them in? Show them how it helps. Start small, get some early wins, and let the results speak for themselves.
Balancing Automation with Human Judgment
Just because the model says a claim might get denied doesn’t mean it always will. It’s still necessary for humans to interpret the data and consider the context. Predictive analytics serves as a powerful tool, but it cannot fully replace human judgment.
The Future of Denial Management: Smarter, More Predictive, and Automated
Here’s where things are headed, and it’s looking a whole lot smarter than before. Denial management analysis used to be a game of catch-up, but now? It’s shifting toward tools that help you get it right before anything even goes out the door.
We’re talking about software that uses AI, real-time claim scrubbing, and natural language processing (NLP) to catch mistakes while you’re still working on the claim. These tools can spot a missing modifier or outdated code and nudge you to fix it right then and there.
And with so much care happening outside the exam room now (telehealth, remote monitoring, even wearables) it only makes sense that billing systems need to catch up. The tools of tomorrow need to handle all of it, and do it without making your team jump through hoops.
Conclusion
Claim denials aren’t going away, but predictive analytics gives you a way to stay ahead of them.
You don’t need to reinvent your whole system overnight. Start with the data, focus on one pain point, and grow from there. The more proactive you are, the more control you have over your revenue.
And in healthcare, that kind of control can make all the difference.
If you’re ready to talk strategy or want help simplifying your denial management analytics, reach out to us at HelpSquad. We’d love to support your journey toward smarter, faster, and more efficient revenue cycle management.
What is denial management in healthcare revenue cycle management (RCM)?
Denial management is the process of preventing, tracking, appealing, and resolving insurance claim denials so providers can collect the revenue they’re owed. It includes identifying why claims were denied, fixing errors, resubmitting claims, and improving workflows to reduce future denials.
Why are claim denials such a big problem right now?
Because they drain revenue and time. Denials slow cash flow, force teams into repetitive rework, and can limit resources available for patient care. Even “small” denial rates add up fast when you’re processing high claim volumes.
What are the most common reasons claims get denied?
The article highlights frequent causes like missing or incorrect codes, outdated documentation, eligibility mismatches, missing attachments, and payer rule changes. These issues often happen at the front end of the process and cascade into bigger delays later.
What is predictive analytics in denial management?
Predictive analytics uses historical claims data, payer behavior, documentation patterns, and other variables to estimate which claims are likely to be denied before submission. It’s designed to flag risk early so teams can correct issues proactively.
How is predictive analytics different from traditional denial reporting?
Traditional reporting tells you what went wrong after the fact. Predictive analytics helps you act ahead of time by identifying denial risk in real time, showing likely root causes, and helping teams fix issues before claims go out the door.


