Remote Patient Care Coordinator: Roles, Skills, and Best Practices
20 Aug 2025 By: Mary Dellosa
Updated
A remote patient care coordinator is a healthcare professional who manages a patient’s medical journey from a distance to ensure care remains steady and connected. These specialists bridge the gap between patients and doctors by monitoring health data from home devices, scheduling virtual visits, and explaining complex treatment plans. For example, a coordinator might review daily blood pressure readings from a patient’s home cuff and alert a physician immediately if the numbers show a dangerous trend.
Hospitals, clinics, and insurers fund remote care since it cuts unneeded stays, manages long-term illness, and backs health programs. A remote patient care coordinator guides each step of care from first contact and review, through steady checks and teaching, to urgent support and handoff when needed.
Core Roles and Responsibilities
A remote patient care coordinator handles many role. Key tasks include intake, triage, care plans, follow-up, risk checks, and team coordination. They use live chat, delayed messages, and data from remote devices.
Duties cover booking telehealth visits, reviewing patient reports, and reading home device data to act when alerts show decline. They also track records, explain meds and care steps, and help with social needs like rides and food.
Patient Assessment and Triage
A main duty is checking a patient’s needs from afar. A remote patient care coordinator use forms, symptom lists, and history checks to judge urgency and care paths. This step spots high-risk patients who need fast review and guides stable ones to remote tracking or learning tools.
Care Plan Implementation
Carrying out and tracking care plans sits at the core of this role. A remote patient care coordinator gives patients clear steps, meds, and tools, then check if they follow them. For long-term illnesses like diabetes, heart failure, or COPD, they use set rules to shift support as patients improve or data shifts.
Coordination and Communication
A remote patient care coordinator makes sure everyone caring for a patient stays connected. They help with referrals, share updates, and remind teams to follow up. By keeping notes clear, they stop things from slipping through the cracks.
Essential Skills and Competencies
A remote patient care coordinator blends medical know-how, comfort with tech, and strong people skills. They explain care in simple words, use telehealth tools with ease, and keep patients and care teams connected.
They also listen with empathy, solve problems, and respect each person’s background. Coordinators look at real-life needs like money, food, or transport, and adjust care to fit. Staying organized helps them give steady, reliable support.
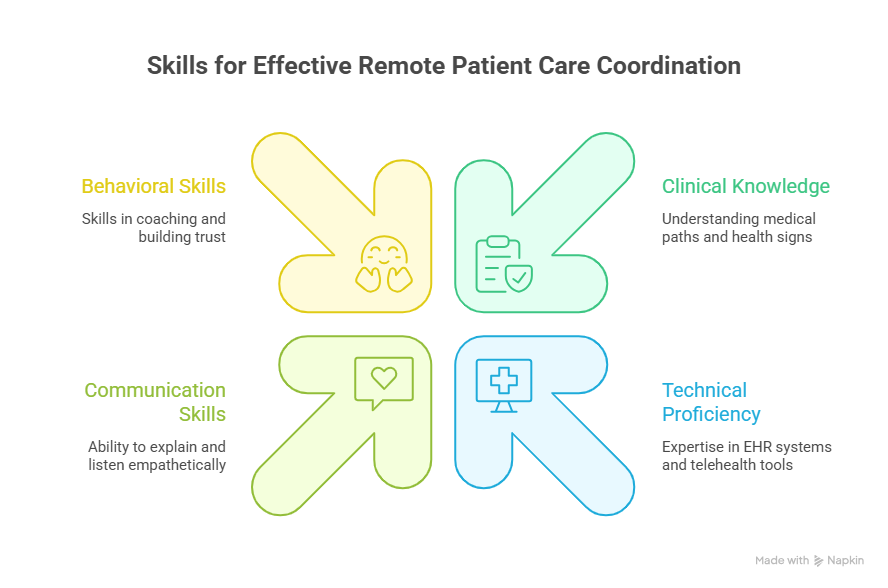
Clinical Knowledge
A remote patient care coordinator don’t always need to be clinicians, but many have medical training. Knowing care paths, medicines, and how to read basic health signs helps them make good choices. Nursing, medical assistant, or case management certificates add strong value. Pursuing RN continuing education courses can also help professionals stay updated on evolving care standards and patient management practices.
Technical Proficiency
A remote patient care coordinator is expected to know EHR systems, telehealth tools, and patient portals. They help fix common tech issues, guide patients with app setup, and read data from home devices like blood pressure cuffs or glucose meters.
Communication and Behavioral Skills
Good coordination starts with kind, clear talk. Using coaching skills and plain words helps patients feel heard and ready to act. Listening with care builds trust, which makes patients more likely to follow their plans and stay involved.
Daily Workflow of a Remote Patient Care Coordinator
A remote patient care coordinator’s day can shift, but some steps stay the same. Most start by checking dashboards and alerts to see which patients need care. Then they reach out by phone or video to check in, teach, and guide. The rest of the day often goes to notes, care plan updates, and quick team meetings.
They balance planned check-ins with sudden alerts that need fast action. Clear steps and triage rules help set priorities. Blocking time for notes and follow-ups keeps care steady and nothing slips through.
Morning: Dashboard Review and Prioritization
Most mornings start with a dashboard that shows patient data, device alerts, and messages. This helps a remote patient care coordinator spot urgent cases and set the day’s focus. They flag serious issues for doctors and plan calls or check-ins for patients who are stable.
Midday: Patient Outreach and Follow-ups
Midday is usually for scheduled calls or video visits. A remote patient care coordinator checks symptoms, review medicines, and share education. They make sure patients understand, help with barriers, and call in a doctor when needed.
Afternoon: Documentation and Team Coordination
Afternoons often focus on paperwork and teamwork. A remote patient care coordinator updates records, write care notes, share follow-up needs, and order supplies or referrals. Team huddles with doctors and social staff keep everyone on the same page.
Tools and Technologies That Empower Coordinators
Many tools make remote care work well. Video visit platforms, patient apps, health records, care software, and home devices all link to give a full view of health. Easy-to-use systems that share data smoothly save time and boost value.
Automation tools handle tasks like alerts and workflows, so coordinators can focus on people. Charts and trends show who may need extra help. Secure, HIPAA-safe messaging keeps care fast while protecting privacy.
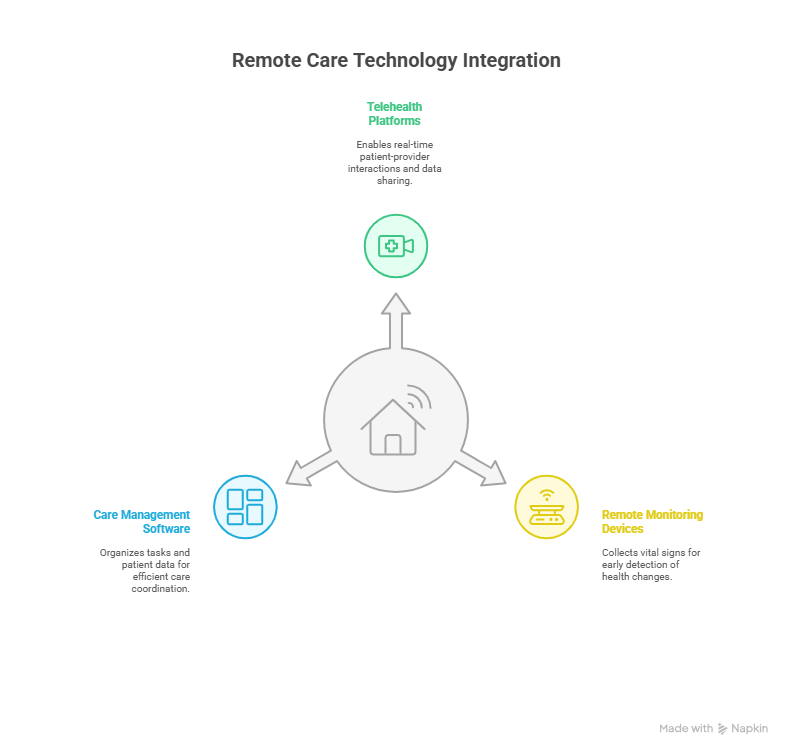
Telehealth and Video Platforms
Strong telehealth tools let patients meet with providers in real time and connect with health records. They should be easy to use, allow note-taking during visits, and share learning materials. Video must run smoothly, with phone calls as a backup when internet is weak.
Remote Monitoring Devices and IoT
Home devices that send vital signs are key for remote care. Tools like blood pressure cuffs, oxygen checkers, scales, and glucose meters spot early changes. Coordinators watch the trends and step in when numbers cross safe limits.
Care Management Software and EHR Integration
Care management tools keep work organized with task lists, risk levels, and patient lists. Linking with health records prevents double work and keeps doctors updated. Dashboards show each coordinator what to focus on so they can manage patients smoothly.
Strategies for Effective Patient Communication
Good communication is the core of remote care. Coordinators use clear scripts, ask patients to repeat key points, and reach out by phone, text, email, or app. Messages shaped for culture and language build trust and understanding.
When many team members talk with a patient, notes should show past talks and next steps. Sharing the same message avoids confusion. Kindness with clear guidance helps patients take an active role in their care.
Teach-Back and Plain Language
Teach-back is about making sure patients feel confident. You ask them to explain the steps in their own words, like telling the story back. If something is unclear, it’s a chance to guide with kindness, not test them. Simple, everyday words keep care easy to follow and help patients feel safe and supported.
Multimodal Outreach and Accessibility
Not everyone likes the same way of staying in touch. Giving choices like phone, text, secure messages, or video makes care easier to reach. It also helps to offer translation, bigger print, or formats for people with vision or hearing challenges, so no one is left out.
Documenting Conversations and Care Decisions
Good record-keeping is key in care. Notes in the health record should capture what was discussed, choices made, and the next steps with clear roles and timelines. This keeps care smooth for patients and protects everyone by meeting legal standards.
Engaging Patients and Boosting Adherence
Engagement isn’t just about staying in touch. It’s about helping patients believe their care plan can really work for them. Coordinators listen, set goals that feel realistic, and teach in ways that fit each person’s life. Small wins, step by step, often build the biggest changes.
Seeing progress makes a big difference. Simple charts showing blood sugar getting better or steady weight loss can spark hope. In some programs, small rewards also give patients an extra push to stay on track.
Setting Realistic Goals
Strong goals feel clear and doable. Setting them together helps patients feel in charge and see real progress. Instead of a vague “eat healthier,” a heart patient might try, “track my meals and lower salt three days a week for one month.” It’s small, specific, and gives a real chance to celebrate success.
Behavioral Techniques and Motivational Interviewing
Motivational interviewing helps patients work through mixed feelings and find their own drive to change. By asking open questions, listening with care, and offering encouragement, coordinators help patients see their own reasons for change and choose steps that match what matters most in their lives.
Measuring Success: Metrics and Quality Indicators
Measuring remote care means looking at both health results and the patient’s experience. Key signs include fewer hospital visits, better medicine use, improved numbers like blood sugar, and higher patient satisfaction.
It also helps to track how fast teams answer alerts, how often check-ins happen, and how well notes get done on time. Using this data to keep improving makes sure care grows stronger and fills gaps.
Clinical Outcomes
The real test of a program is how it improves health. Fewer hospital stays, better control of long-term conditions, and fewer sudden flare-ups show coordination is working. Watching these results over time also proves the program is worth the investment.
Patient Experience and Engagement Metrics
Patient feedback shows how well a program is working. Surveys, ratings, and app use give a snapshot of engagement. Talking directly with patients in interviews or groups offers deeper insight into what helps and what gets in the way.
Operational Metrics
Operational measures show how smoothly a program runs. They include how fast alerts get answered, how many patients each coordinator supports, and how many care plans are finished. These numbers help leaders decide on staffing, tools, and ways to improve daily work.
Best Practices and Protocols
Strong programs blend solid medical steps with care that puts patients first. Clear plans for urgent needs, proven treatment guides, and smooth handoffs reduce errors. Ongoing training helps coordinators stay current with both clinical and tech skills.
Getting a remote patient care coordinator involved early — like right after a hospital stay or new diagnosis — builds steady support and lowers risks. Linking with community resources, such as food or housing help, tackles real-life issues that affect health.
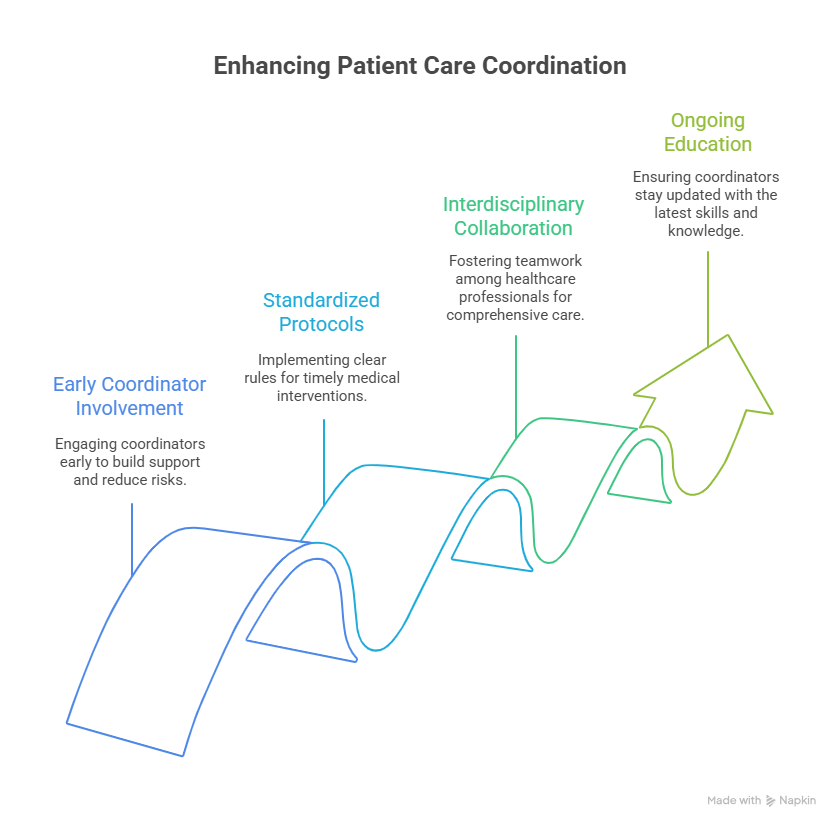
Standardized Escalation Protocols
Clear rules for when to call in a doctor help avoid dangerous delays. These steps should be proven, simple to follow, and fit each condition. Standard notes and messages make sure the whole team stays on the same page and responsible for next steps.
Interdisciplinary Collaboration
Coordination works best when the whole team shares responsibility for a patient’s health. Regular case reviews, joint planning, and shared goals bring doctors, pharmacists, social workers, and community partners together to give patients stronger, more connected care.
Training and Ongoing Education
Learning never stops for coordinators. Staying current on health updates, cultures, and new tech helps them support patients better. Role-play and practice sessions give them confidence for tough situations. Earning certificates in care or telehealth shows patients they are in skilled, trusted hands.
Common Challenges and Practical Solutions
Remote care isn’t without challenges. Some patients struggle with tech or don’t have access. Too many alerts can overwhelm teams, and patients may feel tired of constant check-ins. Programs need to plan ahead, design with patients in mind, and keep workflows flexible.
Solutions can be simple. Offer phone calls for those without smartphones. Set smart filters so alerts really matter. Focus support on patients who need it most. Most of all, steady, kind communication builds trust and helps patients feel safe with remote care.
Technology Barriers
Not every patient has strong internet or the right device. Loaner programs, simple apps, and phone options help close this gap. Clear training and easy step-by-step guides make setup less stressful and give patients confidence to stay connected.
Alert Fatigue and Data Overload
When too many alerts pop up, real problems can get overlooked. Smarter systems sort the noise and bring the urgent signals to the front. This way, care teams can act quickly, and patients know their most important needs won’t be missed.
Maintaining Patient Engagement Over Time
Living with sickness every day can be tiring. It helps when plans get refreshed, small steps are praised, and family or friends give support. When care feels simple and made for real life, it feels lighter and gives hope to keep moving forward.
Legal, Privacy, and Reimbursement Considerations
Remote care has to keep patients safe and their information private. That means using secure messages, getting clear consent, and storing data safely. How programs are paid for — by each visit, by overall results, or in bundles — affects how they are designed and how long they last.
Good records not only meet the rules but also show the value of care. Coordinators learn the right billing codes for remote check-ins and long-term support so patients can keep receiving the services they need.
Data Privacy and Security
Patient privacy matters most. Safe messages, easy device setup, and limited access keep details protected. Regular checks and staff training add safety. Clear forms explain how data is used, so patients can feel calm and trust their care.
Reimbursement Models
Paying for remote care is changing. More programs now reward good results and fewer hospital visits, which fits well with remote coordination. In places that still pay per service, knowing the right billing codes for check-ins and monitoring helps keep programs running.
Career Path and Professional Development
A career as a remote care coordinator can grow in many directions. You might step into leadership, manage health programs, or focus on areas like cancer, heart care, or mental health. These paths bring more responsibility and a bigger role in guiding care.
Learning never stops. Gaining certifications in case management, telehealth, or quality improvement helps you move forward. When coordinators show real results and better patient outcomes, it opens doors to leadership and new opportunities.
Advancement Opportunities
Career growth can take many paths. Coordinators may become senior coordinators, team leads, or supervisors. Others move into program design or data work. Some choose teaching, health technology, or policy roles that shape how remote care is delivered.
Skills for Growth
Certain skills help coordinators grow in their careers. Project management, data skills, quality improvement, and leadership all open new doors. Knowing how to use analytics tools and read metrics lets coordinators improve programs and take part in bigger planning.
Trending Now
Burnout in healthcare workers lowers care quality and harms both staff and patients. Stress, long hours, and poor support drain energy and reduce empathy. This leads to more errors, weak communication, and patient dissatisfaction. Burnout also worsens patient outcomes and delays healing. Supportive work settings, better training, and stress relief plans can protect health staff and improve care.
Conclusion: The Future of Remote Patient Care Coordination
Remote care coordination is becoming a trusted part of healthcare. With better tools, coordinators can stay close to patients, work side by side with doctors, and give support that feels personal and kind.
At its core, this work is about people. Coordinators bring knowledge, compassion, and clear guidance. When programs listen to patients and care for staff, everyone benefits — patients feel safe and supported, providers feel confident, and the health system grows stronger for all.
HelpSquad Health goes beyond 24/7 live chat to offer full healthcare outsourcing services. Our trained team supports providers with patient outreach, care coordination, and administrative tasks, helping reduce workload and improve efficiency. Partner with HelpSquad Health to give your patients seamless, compassionate support while your team focuses on what matters most, quality care.