Adapting Billing Workflows to Value-Based Care Models in 2025
29 Jul 2025 By: Maria Rush
Updated
In 2025, value-based care means providers get paid based on patient outcomes, not just the number of services delivered, so billing workflows must connect clinical results to reimbursement. Billing teams need data flowing between the EHR and revenue systems to capture quality metrics, risk adjustments, and performance thresholds. For example, tracking fewer readmissions or better diabetes control can directly affect shared savings or bonus payments, so documentation and reporting have to be consistent and timely.
What is Value Based Care?
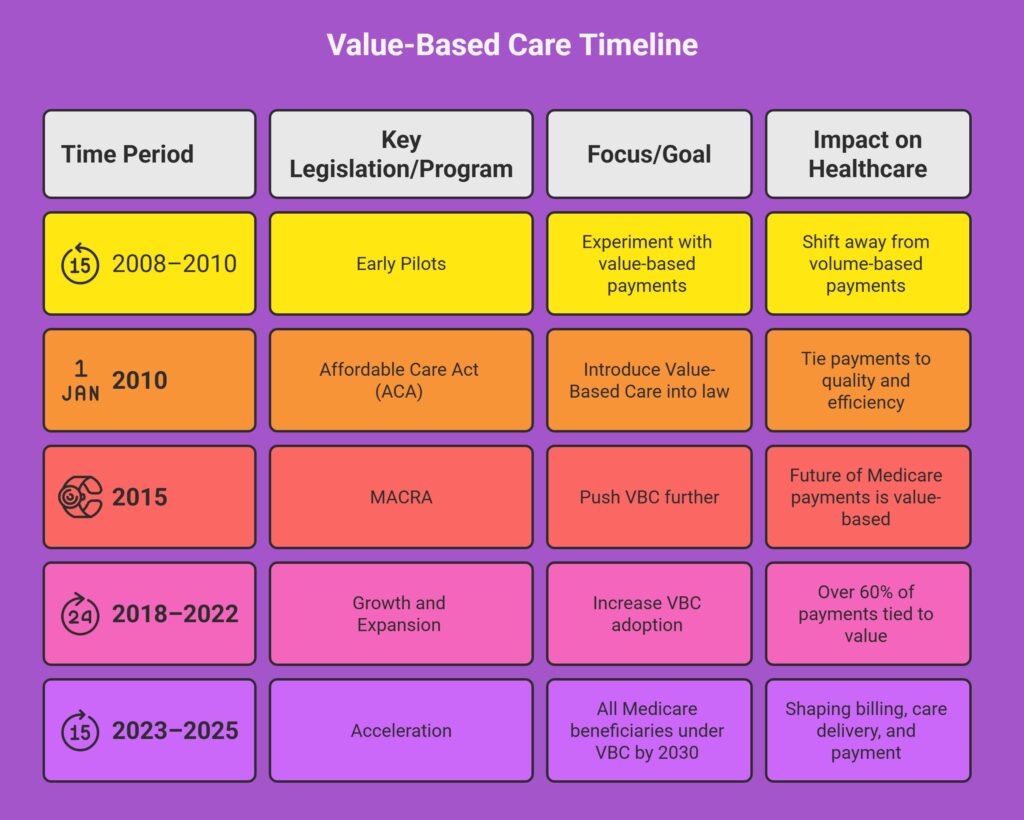
Value-based reimbursement shifts the focus from volume to results. Instead of paying providers for each test or procedure, payers are looking at how well patients are doing. Things like fewer ER visits, better chronic care management, and shorter hospital stays all factor into how payments are calculated.
Programs like Medicare’s Shared Savings and Quality Payment Programs are leading this change. And commercial insurers are following suit.
By the end of 2023, over 60% of U.S. healthcare payments were tied to value-based arrangements. CMS wants most Medicare beneficiaries covered under these models by 2030.
To succeed in this healthcare model, providers need systems that can track performance, document outcomes, and align billing with clinical operations. The ability to connect care quality to reimbursement is now essential.
Fee for Service VS Value Based Care
Most billing systems were built for fee-for-service. They’re focused on volume, getting the codes right, submitting the claim, and getting paid. But value based care is more complex. You’re dealing with quality metrics, risk adjustments, care episodes, and performance thresholds.
These older systems struggle because:
- They don’t connect with clinical outcomes or track quality benchmarks.
- They can’t manage new payment models like bundled payments or shared savings.
- They rely too much on manual entry and are prone to errors that lead to denials.
Worse, when billing and clinical data live in separate systems, it creates delays, confusion, and missed opportunities for better reimbursement. Nowadays, that kind of disconnect can cost you.
Read more related articles:
Healthcare BPO Market Growth
The Impact of Medical Healthcare Call Centers
Healthcare IT Outsourcing
What Needs to Change in 2025
If your practice wants to get paid for the care you’re already providing, a few things need to change:
- Data needs to flow between clinical and billing systems. This ensures you’re capturing the outcomes needed for value-based reimbursement.
- Smart technology and automation should really be considered. Tools that can predict denials, catch coding gaps, and track performance are no longer nice-to-haves.
- Your team needs training. Everyone—from clinicians to billing staff—should understand the metrics that affect payments.
Some health systems using AI and predictive tools have cut denial rates by up to 40%. Practices that invest in these tools and team alignment now will be better positioned as the system continues to evolve.
Trending Now: Better Data = Better Value-Based Care
A recent article from Health Affairs points out that value-based care can’t work without better data. Many providers still rely heavily on ICD-10-CM codes, which don’t capture enough clinical detail. That makes it harder to measure outcomes, costs, and quality accurately.
The article suggests moving to improved coding systems like ICD-11 with its clinical extension or using frameworks like SNOMED CT, which already capture richer clinical data. Better data means stronger risk adjustment, more accurate claims, and better analytics. These are key pieces needed to make value-based care truly effective.
The Role of Outsourced Billing Partners in the Value-Based Care Model
This is the part many providers overlook, but it’s one of the smartest changes you can make.
Handling value-based billing in-house can be overwhelming. Payer rules keep changing, and new models require constant updates to documentation, coding, and reporting. That’s why outsourced billing partners are more in-demand than ever.
They’re not just here to submit claims. A good partner brings:
- Expertise in value-based reimbursement. They are familiar with the metrics, coding, and payer expectations.
- Technology integration. The best partners use platforms that link directly to your EHR and pull in relevant clinical data.
- Compliance coverage. They stay updated on CMS and commercial payer requirements.
- Denial prevention and appeals support. They can flag potential issues before claims go out, and recover lost revenue when denials happen.
- Analytics and insights. A strong billing team doesn’t just manage your revenue—they help improve it with real-time performance feedback.
The global RCM outsourcing market is projected to reach $116 billion by the end of 2025. That’s not just hype. It reflects how providers are responding to staffing shortages, rising admin costs, and the growing complexity of billing.
When done right, outsourcing doesn’t just ease the load. It helps you get ahead. And in a payment system that rewards outcomes, speed, and accuracy, that kind of support makes all the difference.
How HelpSquad Supports the Shift
At HelpSquad, we work with practices that want billing to be less stressful—and more aligned with the care they provide. We combine skilled billing support, AI-backed tools, and responsive training to help providers:
- Reduce denials and resubmissions
- Capture value-based payment opportunities
- Stay current on compliance and reporting
- Keep billing teams and care teams on the same page
We also offer patient-friendly billing communication. Because transparency builds trust, and that’s part of what value based care is all about too.
Final Thoughts: Billing for Outcomes, Not Just Services
Value-based care ties your financial health directly to how well your patients do. Clear documentation, accurate data, and strong coordination between teams are now essential.
Billing processes must reflect patient outcomes. Data needs to be timely and accurate, reports must show measurable results, and quality metrics should be tracked consistently. When billing and clinical teams work together, it becomes easier to meet payer requirements and keep revenue stable.
Focusing on outcome-based billing isn’t just about compliance; it supports better care for patients and ensures your practice can continue to grow.
Want to learn more about how to strengthen your billing process for value-based care?
Talk to us. We can help you make sure your billing supports your patients and your practice.