Understanding the Cost of AI in Healthcare
16 Aug 2025 By: Vlade Legaspi
Updated
The cost of AI in healthcare includes far more than a license or cloud subscription. Healthcare teams often pay for data cleanup and labeling, model development and validation, compute infrastructure, integration with EHR workflows, compliance and legal review, staff training, and ongoing monitoring to prevent performance drift. For example, a hospital may spend heavily on preparing imaging or EHR data and running clinical validation before the AI tool can be safely used in daily care.
Why cost matters: clinical promise versus financial reality
Health systems face thin margins and tough rules. The artificial intelligence healthcare cost must prove value or risk wasting funds without better results. Leaders must see where money goes, how gains show, and how spending boosts care or efficiency.
Leaders also weigh trade-offs: funding one AI project means less for staff, services, or sites. A clear look at costs and gains ensures AI use stays fair, smart, and in line with goals.
Breaking down the cost categories
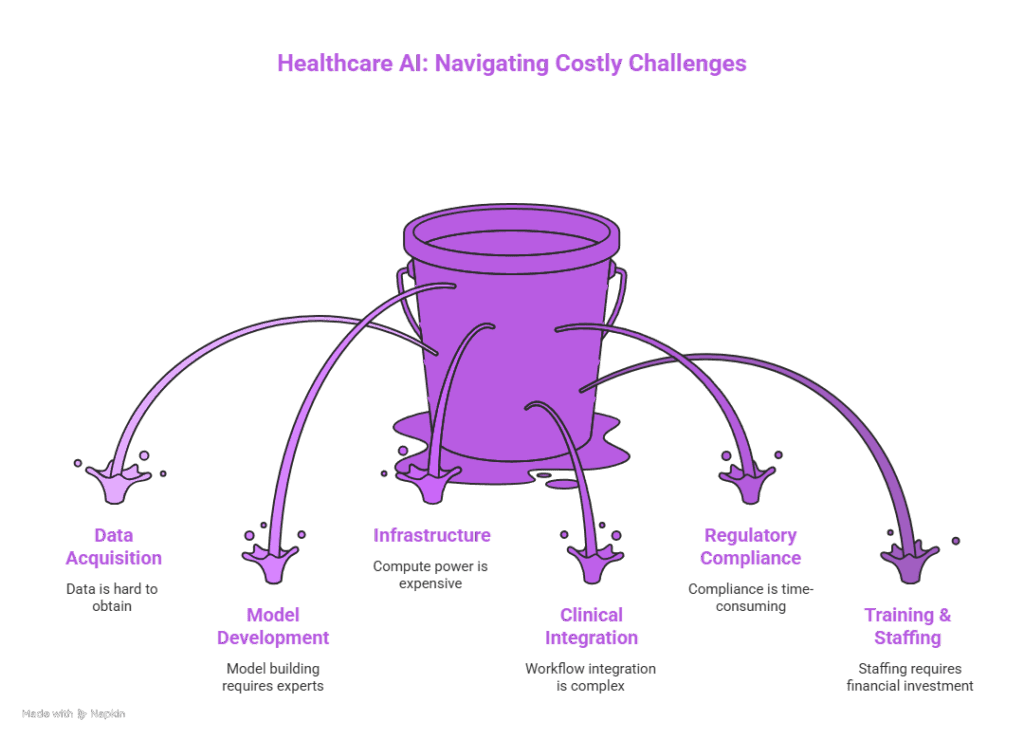
AI spending in healthcare falls into key groups. Each brings direct and hidden costs that shape the total cost of AI in healthcare. Knowing these groups helps plan, spot risks, and set priorities.
Main cost areas include data setup, model build and test, system fit, workflow link, rule checks, staff training, upkeep, and insurance. Each shifts based on use and group size.
Data acquisition and curation
Strong data drives any AI system. Health groups often merge records, scans, labs, and patient data. The cost of AI in healthcare grows with extraction, cleaning, and labels, often needing doctors to check and mark.
Extra costs come from buying datasets, using platforms, and adding rules to guard privacy. Time and work to fix gaps, match terms, and update old systems can rise fast, especially across many sites.
Model development and validation
Building AI models needs experts like data scientists, engineers, and doctors. The cost of AI in healthcare rises with model design, tests, and doctor input for labels.
Strong checks are vital for safety and approval. Trials and site studies cost more and take time. Wider testing adds cost but lowers risk across groups and settings.
Infrastructure and compute
AI work needs strong compute power for training and use. The cost of AI in healthcare climbs with GPU clusters or cloud tools, plus real-time system demands.
Groups must weigh local gear, hybrid, or cloud setups. Hardware costs shift to cloud fees, which rise if unmanaged. Backup and data rules also shape spend.
Integration with clinical workflows
The implementation of an AI tool in a clinical environment requires more than the algorithm since it needs to blend seamlessly with EHR systems as well as picture archiving and communication systems (PACS) and laboratory systems and clinician workflows. Integration costs include API development, middleware, user interface design, and extensive testing to ensure the AI output is accessible and actionable at the point of care.
The improper integration of systems results in decreased adoption rates and clinician dissatisfaction and operational blockages. Human-centered design and clinical end-user testing require mandatory implementation and planning should allocate funds for usability testing and clinician time and iterative engineering efforts.
Regulatory, legal, and compliance costs
AI in Healthcare falls under regulatory control and different jurisdictions apply their own rules based on the specific use of AI systems. The process of obtaining regulatory clearance or approval requires substantial time and expense for clinical evidence generation and documentation and regulatory body liaison. The post-market surveillance requirements demand continuous data collection together with reporting duties.
The legal framework includes several components that need to be considered such as contracts and data-sharing agreements together with intellectual property rights and liability protection. Organizations must invest in legal counsel and compliance officers and secure processes to meet privacy regulations including HIPAA and GDPR which adds costs for protecting patient confidentiality and institutional risk profiles.
Training, change management, and staffing
The implementation of AI technology in healthcare facilities demands financial investment for staff training along with changes in operational procedures. The healthcare workforce requires training to understand AI output interpretations and learn when to follow suggestions and how to record decisions influenced by AI systems. The costs include programs for training and educational resources and continuous support services.
The implementation of change management requires clinical champions along with workflow alignment and possibly role redefinition through the establishment of AI governance committees and new informatics positions. Organizations face competitive challenges when trying to recruit and retain staff who possess AI expertise which may necessitate higher salaries or alternative incentives for their workforce. In these cases, some health systems turn to healthcare it recruiting firms to speed up access to experienced specialists without overloading internal HR teams or delaying AI initiatives.
Monitoring, maintenance, and model drift
The deployed models require continuous monitoring to detect both performance decline and changes in the dataset. The ongoing operational expenses result from monitoring infrastructure combined with periodic retraining and performance audits and incident response processes. The oversight of safety-critical applications must remain continuous because it is non-negotiable.
The costs of maintenance include software updates and model adaptations to keep up with clinical guidelines and reimbursement policies changes. The requirement to train models with fresh labeled data repeatedly leads to increased long-term costs and small model updates may trigger additional validation steps and regulatory reporting requirements which increase expenses.
Insurance and liability
The emerging concern in medical practice involves the potential risks of AI-related malpractice. The need for liability coverage expansion and AI-specific insurance products exists for institutions that want to protect themselves from AI-induced risks. Before insurers provide coverage they demand documentation of governance processes and validation results and monitoring programs which create additional administrative and financial challenges.
The legal risks extend past the realm of clinical damage. The combination of data breaches and IP disputes and vendor contract disputes creates potential expenses from costly legal battles. Both patients and organizations require proactive legal and insurance planning to protect themselves from financial risks.
What are the Major cost drivers and variability?
AI projects exist at different expense levels. The development of predictive models that analyze structured claims data proves less expensive than creating multimodal models which process medical images and genomics data at high resolutions. The clinical risk level together with deployment scale and real-time inference requirements determine the most crucial cost factors.
Healthcare facilities with smaller size must spend more per patient because of their limited operational scale although large health systems can distribute their fixed costs throughout multiple facilities and patient populations. The final cost of a project depends on geographic elements which include labor market salary norms and regulatory complexity as well as the availability of cloud infrastructure.
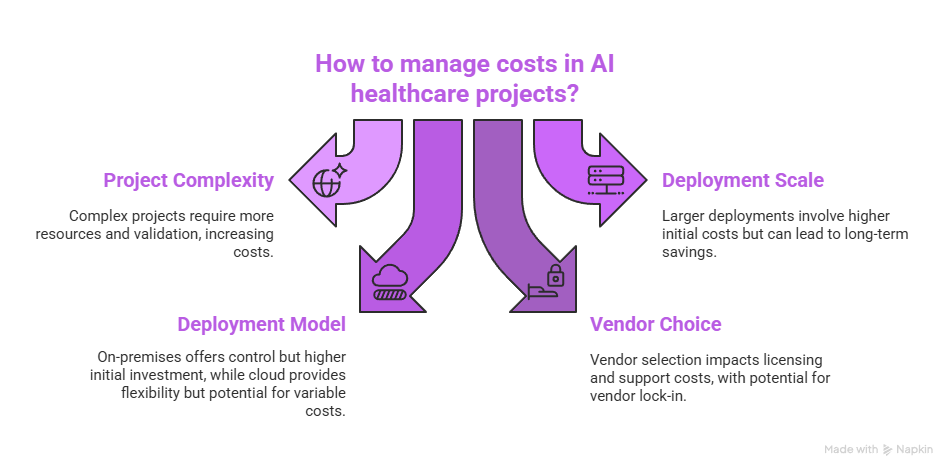
Scope and complexity of the use case
Basic decision-support tools that warn about unusual lab results and handle administrative tasks need minimal data and basic models and straightforward integration which results in lower costs. The development of diagnostic AI systems for radiology and pathology and genomics requires complex models and extensive labeled datasets and rigorous validation procedures that substantially increase costs.
Complex use cases require multidisciplinary teams and extensive clinical trials for their development. The present value of costs and time to break-even both increase as a result of prolonged timelines.
Scale and deployment model
The deployment size determines how much the costs will increase. The cost of implementing an AI tool for one department remains lower than implementing it throughout the entire organization. Successful deployment across the entire system enables shared integration work that benefits different departments and centralized data platforms minimize data duplication.
The deployment model, on-premises versus cloud, affects both capital and operational spending profiles. Large hardware investments at the start of on-premises systems lead to predictable long-term costs and complete control of data. Cloud deployments enable capital expenses to transform into operational expenses but users need to actively control costs to prevent excessive billing.
Vendor choice and licensing models
The choice of vendor determines expenses through licensing models together with support agreements and customization fees. The business model of vendors includes user-based and inference-based fees in addition to subscription-based and outcome-based pricing structures. The maintenance and update fees for proprietary models differ from open-source solutions because the latter require internal engineering and integration expenses for cost management.
Organizations should evaluate vendor lock-in because it generates significant financial consequences in the future. Organizations need to evaluate their contracts for length and exit clauses and data portability requirements to avoid future cost expenses when moving between solutions or system integrations.
Measuring value and ROI
The evaluation of costs requires comparison to specific measurable advantages. AI projects which decrease readmissions and shorten hospital stays and decrease diagnostic errors and boost patient flow generate direct financial benefits and free up capacity to enhance patient care. The value generated by these projects remains challenging to measure because it includes better clinician satisfaction and enhanced patient experience.
The return on investment (ROI) analysis should calculate both direct financial savings and revenue growth and cost reductions which include the prevention of adverse events and resource optimization. The time period affects how benefits materialize because administrative automation produces immediate results but population health improvements take multiple years to develop.
Quantifiable benefits
The implementation of targeted orders for laboratory and imaging tests leads to reduced utilization while faster diagnosis results in shorter hospital stays and automated coding and billing systems boost revenue collection. The implementation of these benefits becomes trackable with reasonable precision through baseline data collection.
The implementation of predictive maintenance for equipment and the reduction of adverse events enables organizations to avoid costs through reduced legal exposure and readmissions. The deployment of AI systems requires pre-deployment baseline metric collection to establish valid ROI measurement.
Intangible and strategic value
AI investments provide organizations with strategic benefits through enhanced reputation and talent acquisition capabilities and research collaboration opportunities. These benefits remain difficult to measure but they affect both financial stability and market position during extended periods.
The implementation of AI technology allows healthcare organizations to create new treatment methods through remote patient monitoring and virtual healthcare services which expand their service capabilities and help value-based care models while generating revenue and improving population health outcomes.
Financing models and procurement strategies
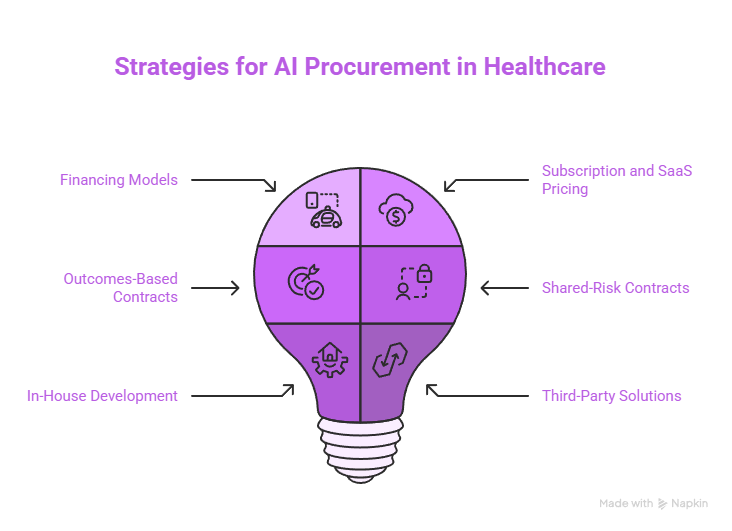
Health systems together with their providers select various funding methods to obtain AI capabilities. The main financing methods used by health systems and providers include upfront capital purchases together with subscription models and pay-per-use and performance-based contracting and public-private partnerships. The selection of financing method depends on financial flexibility together with risk tolerance and strategic priorities.
Academic centers can use grants and research collaborations to reduce their expenses during early-stage development. Leasing hardware together with cloud credits helps organizations reduce their initial financial expenses. The management of long-term costs becomes more effective when vendors create contracts with defined service-level agreements and support services and transparent ai-driven hospital procurement pricing.
Subscription and SaaS pricing
The Software-as-a-Service (SaaS) pricing model reduces initial expenses and transfers maintenance duties to the vendor. The subscription model provides institutions with predictable payments that include automated system updates. The total subscription expenses throughout multiple years might surpass one-time purchase costs so organizations need to evaluate all included features carefully.
The Software-as-a-Service (SaaS) model proves suitable for organizations with limited internal engineering capabilities. The negotiation of user limits and inference quantities and integration support services leads to better institutional needs and budget alignment.
Outcomes-based and shared-risk contracts
The payment structure of outcomes-based contracts links financial compensation to performance metrics which include readmission rate reductions and diagnostic accuracy targets. The incentive alignment between vendors and providers requires established measurement systems and agreed-upon baselines and mutual risk-sharing terms.
Shared-risk contracts drive vendors to invest in implementation and support but create complex accounting requirements while needing strong data sharing systems and governance for reliable outcome measurement.
In-house development versus third-party solutions
The development of AI systems within an organization allows for data control and customization and future adaptability but demands major investments in human resources and infrastructure. The purchase of third-party solutions speeds up deployment while transferring some vendor-related risks but organizations must pay for customization and integration work.
Internal teams that customize open-source models or work with vendors to co-develop solutions can achieve cost-effective and controlled solutions at an optimal speed but need proper governance systems to handle intellectual property and ongoing responsibilities.
What are the Strategies to control and optimize costs of AI in Healthcare?
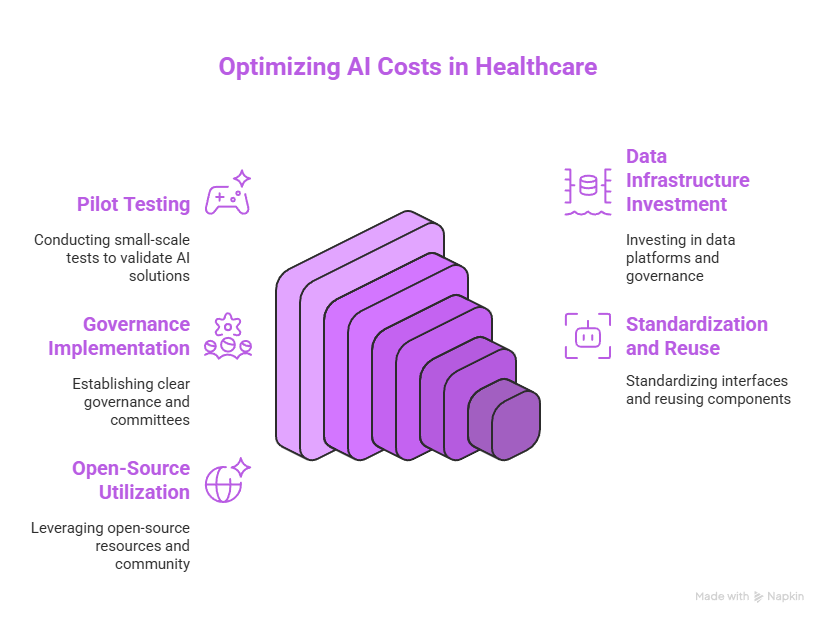
Cost of AI in Healthcare control demands organizations to develop strategic plans and define realistic boundaries and maintain ongoing measurement systems. Leveraging expert guidance such as AI automation consulting can help health systems identify reusable data models, streamline workflows, and avoid costly re-engineering during scale-up.
The combination of small project achievements with repeated pilot tests helps organizations decrease financial exposure while building proof for future expansion. Organizations that make strategic investments in data infrastructure and governance will achieve lower costs because these investments help eliminate duplication and speed up future projects.
The combination of clear governance with cross-disciplinary steering committees and staged rollouts enables stakeholders to align their expectations while preventing costly missteps. The process of benchmarking with peer organizations and studying existing deployments helps organizations avoid repeating typical deployment mistakes.
Start small, scale thoughtfully
The implementation of focused pilots with specific success metrics allows organizations to gain quick learning while minimizing expenses. The testing phase of pilots should evaluate how different components integrate together and how users will receive the system and measure its outcomes. Standardization of interfaces and component reuse after successful pilots leads to lower marginal costs when expanding operations.
The selection of interoperable standards together with modular architectures and reusable data pipelines during initial planning stages prevents organizations from needing costly rewrites and integration projects in the future.
Invest in data platforms and reuse
The establishment of a centralized data platform under proper governance control lowers the expenses associated with data preparation work for individual projects. The implementation of reusable data models together with common ontologies and standardized labeling processes enables faster new project development while minimizing repetitive work between departments.
Data catalogs together with metadata management systems enhance dataset discovery and decrease the time needed to prepare datasets for new AI projects.
Leverage open-source and community resources
The use of open-source models and tools decreases development expenses but requires the buyer to take full responsibility for validation and integration and maintenance tasks. Community benchmarks together with shared datasets help developers shorten their development time while establishing performance comparison standards.
Cost-sharing for data curation and validation activities becomes possible through consortium and collaborative research network participation especially for rare conditions that lack sufficient data at individual institutions.
Ethical, legal, and societal costs of AI in healthcare
AI in healthcare generates financial expenses and ethical and societal implications which affect both long-term sustainability and institutional reputation. The use of biased data leads to increased disparities and the lack of transparency in models damages public trust. The resolution of these problems demands financial support for fairness testing and explainability development as well as stakeholder participation.
All healthcare organizations need to implement proactive ethics and equity review processes because they are not voluntary. These processes need time along with expert resources and sometimes modified data collection procedures to decrease future expenses from harm incidents and legal cases and trust damage.
Addressing bias and fairness
The process of bias reduction demands additional representative data collection and subgroup analysis and model or workflow modifications to stop disparate effects. The initial financial investment in these efforts becomes necessary to stop harm and meet future legal standards.
The inclusion of diverse stakeholders including patient representatives and community groups enhances the validity of AI deployment plans by revealing potential costs and harms that technical teams would miss.
Explainability and transparency
The medical field requires both clinicians and patients to understand how AI systems generate their recommendations. The creation of interpretable models together with the implementation of explainability layers necessitates engineering and design resources. The process of transparency demands documentation together with model cards and accessible summaries that explain both limitations and intended use of the system.
The creation of these materials builds trust and streamlines regulatory assessments yet organizations need to include funding for their development in their deployment plans.
Future trends that will affect costs
Healthcare costs associated with AI will transform because of technological progress and regulatory changes and market fluctuations. The combination of more efficient models and wider pre-trained model availability and better tooling systems will decrease development expenses and computational costs. The combination of stricter regulatory requirements and rising social expectations about fairness and transparency will result in increased costs for compliance.
The vendor ecosystem consolidation process will create standardized interfaces which decreases integration expenses but the competition for AI talent might lead to higher salary expenses. Organizations need to understand these trends to create plans that focus on future developments.
Model efficiency and edge computing
Model architecture improvements along with on-device inference capabilities decrease the need for expensive cloud computing resources and minimize operational costs for applications that need real-time processing. Edge deployments resolve data residency and latency issues but organizations must spend money on device management and security measures.
The availability of more efficient models enables smaller healthcare facilities to access capabilities which were previously available only at large centers thus transforming the cost structure of the entire ecosystem.
Regulatory maturation and standards
The establishment of clear AI approval pathways by regulators will enhance purchasing decision predictability while decreasing compliance uncertainty. The costs of compliance will likely rise because new requirements for transparency and fairness testing and continuous monitoring will become mandatory standards.
Standardization of data formats and APIs will lower integration expenses in the future yet organizations must invest during the transition to new standards.
Trending Now!
The research investigates how artificial intelligence reduces healthcare expenses during diagnosis and treatment operations when compared to traditional medical practices. The increasing medical expenses in the United States demand efficient solutions to address this problem. AI technology delivers precise diagnoses while accelerating medical interventions and minimizing mistakes which leads to financial savings. The research evaluates 200 studies to determine cost-effectiveness in medical fields including cardiology, oncology, dermatology and COVID-19 care. Economic models demonstrate that AI treatment generates superior savings than AI diagnosis throughout the long term. The implementation process demands regulatory clearance together with employee training and FDA standard compliance.
The paper examines three emerging AI trends which include pruning and explainable AI and bias control to boost efficiency and trust. These technological advancements create economic benefits through smaller model sizes and improved clarity and reduced risk factors. The implementation of AI faces ongoing challenges because of infrastructure expenses and data requirements and regulatory obstacles. The research demonstrates that AI exists to assist medical professionals instead of replacing them. AI needs to demonstrate cost-effectiveness while building clinical trust and obtaining regulatory approval to achieve success. The correct implementation of this technology enables the development of sustainable healthcare systems which are both fair and efficient across the world.
Conclusion: budgeting for realistic and sustainable AI
The research demonstrates that AI technology reduces healthcare expenses during diagnosis and treatment procedures when compared to traditional diagnostic approaches. Better solutions are needed to address the increasing medical expenses in the United States. AI technology enhances both the speed of medical care and diagnostic precision and reduces mistakes which leads to cost reductions. The analysis of 200 studies demonstrates how AI delivers cost advantages across cardiology and oncology and dermatology and COVID-19 treatment. The models demonstrate that AI treatment produces greater savings than diagnosis does in the long term. The success of AI depends on three essential factors which include training programs and FDA approval and clinical suitability.
The study examines current trends including pruning and explainable AI and bias checks which enhance trust and operational efficiency. The advances lead to smaller model sizes and better clarity and reduced risks. Several challenges persist because of high costs and strict rules and data usage limitations. AI technology exists to assist doctors in their work rather than replace them. The system needs to demonstrate financial savings and gain trust from patients and meet established standards to succeed. AI systems produce fair and efficient and lasting care systems when properly implemented.
To experience these benefits firsthand you should join Helpsquad Health right now. Begin your free trial to discover how AI technology reduces expenses while enhancing medical care for patients. Your healthcare system needs transformation so you should not pass up this opportunity.
Why is the cost of AI in healthcare such a big deal right now?
Because health systems run on thin margins and strict regulations. AI has real clinical promise, but the cost of AI in healthcare must clearly translate into better outcomes, faster workflows, fewer errors, or measurable savings, otherwise it becomes an expensive experiment that doesn’t improve care.
What makes up the total cost of AI implementation in healthcare?
The total cost of AI in healthcare goes well beyond licensing or cloud fees. It typically includes data acquisition and preparation, model development and validation, infrastructure and compute, integration with EHR/PACS/workflows, regulatory and legal compliance, staff training and change management, ongoing monitoring and maintenance, and insurance/liability planning.
Why is data acquisition and curation often one of the biggest cost drivers?
Healthcare AI needs high-quality data from EHRs, imaging, labs, and other sources. Costs rise quickly from extracting data, cleaning it, standardizing formats, resolving gaps, protecting privacy, and labeling data, often requiring clinician time to review and annotate.
What costs are involved in model development and validation?
Building and validating AI models requires specialized talent (data scientists, engineers, informaticists) plus clinician involvement. Validation is expensive because safety matters: rigorous testing, site studies, and evidence generation are often needed, especially for higher-risk clinical use cases.
How do infrastructure and compute costs show up in healthcare AI budgets?
AI systems can require significant compute for training and real-time inference. Whether you choose on-prem GPUs, cloud, or hybrid, you’ll still face costs tied to performance needs, storage, backups, data residency requirements, and the risk of runaway cloud spending if usage isn’t managed.


