Claims Denial Management in 2025: Best Practices, Tools, and Trends
05 Aug 2025 By: Maria Rush
Updated
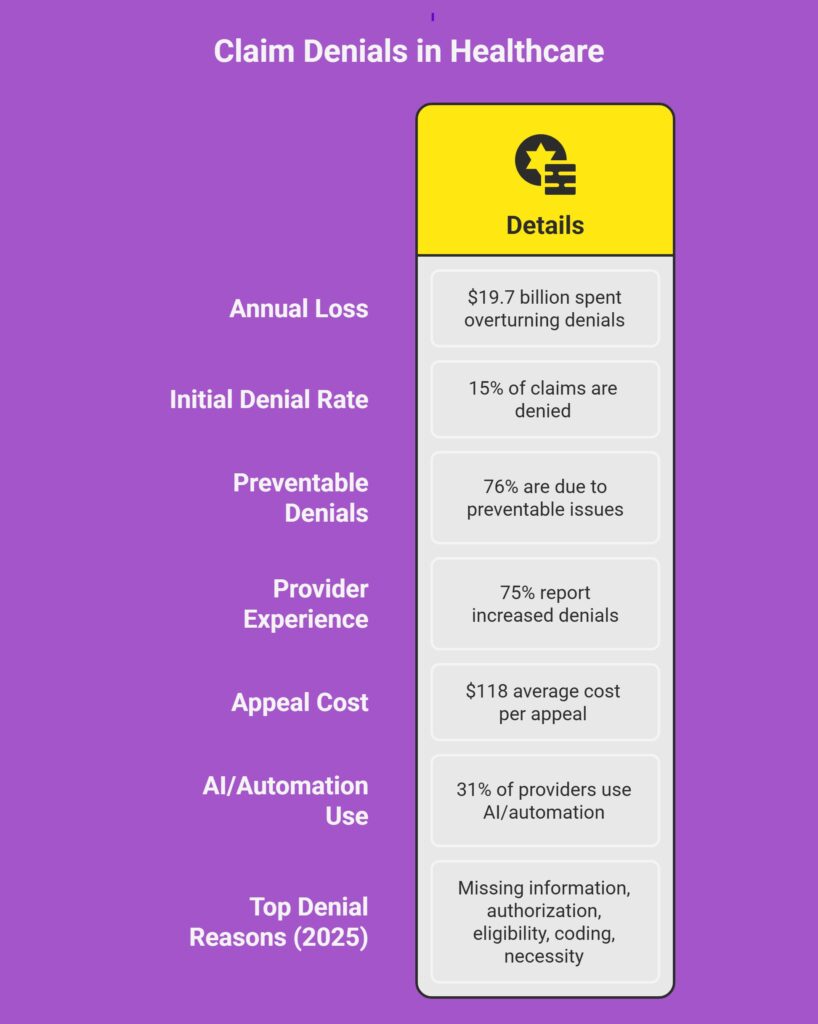
Claim denials are a massive headache. They slow down payments, eat up staff time, and cost hospitals and clinics billions.
So what’s really going on? In my experience as someone who worked in healthcare, the old approach to claims denial management just does not work anymore. Reacting after a denial hits is expensive and exhausting. What actually moves the needle is prevention. Fixing root causes, tightening workflows, and using smarter systems so claims do not get rejected in the first place. For a lot of healthcare teams, that also means bringing in outside support like HelpSquad when internal teams are already stretched thin.
What are the Best Practices in Claims Denial Management?
Clean Claims from the Start
Most denials can be avoided. I know that sounds optimistic, but the data backs it up. Studies show that up to 76 percent of denials happen because of missing or incorrect information. That is why strong claims denial management always starts with clean claims. It is one of the most overlooked hospital denials management best practices.
Real-Time Insurance Verification
This starts before the visit even happens. Real-time insurance verification at intake helps catch issues early. Wrong payer, inactive coverage, missing authorization, all of that can be flagged upfront. From a healthcare claims denial management perspective, this step alone prevents a surprising number of downstream problems.
Solid Documentation and Coding
Documentation is where many claims fall apart. If the notes do not support the codes, denials are almost guaranteed. I have seen teams reduce denials simply by tightening documentation standards and using claims rejection management tools that flag mismatches before submission. Ongoing coder training matters more than most teams realize.
A Proactive Mindset
The biggest change I see in high-performing teams is mindset. Instead of chasing denials after they happen, they focus on stopping them upstream. Front desk teams understand payer rules. Deadlines are respected. EMRs are set up to catch issues early. This proactive approach is a core part of hospital denials management best practices today.
Predictive Analytics in Action
Predictive analytics is becoming a real advantage. With enough historical data, some systems can now flag high-risk claims before submission. Think of it as an early warning system. Teams can double-check documentation or add supporting notes in advance. automated claims denial management plays a big role here, especially when teams are managing high volumes.
When Denials Still Happen (Because They Will)
Track, Categorize, and Analyze
Even with the best setup, denials still happen. That is reality. What matters is how fast and clearly you respond.
Strong claims denial management means tracking every denial and understanding why it happened. Missing documentation, coding errors, authorization gaps, all of it should be categorized. Modern claims rejection management tools make this easier by showing patterns that would otherwise be missed.
Swift Denial Resolution Workflow
Speed matters. A good denial workflow assigns ownership quickly and works denials within days, not weeks. Claims go into a worklist, corrections are made, and appeals are submitted on time. Miss the filing window and the revenue is gone. automated claims denial management helps teams stay on top of deadlines without relying on memory.
The Power of Outsourcing
This is where outsourcing can make a real difference. Not every organization has the bandwidth to manage denials internally. A partner like HelpSquad can step in, work directly inside your system, and support healthcare claims denial management without adding pressure to your internal staff.
Denial Management Tools That Make All the Difference
Claim Scrubbers
Claim scrubbers are now a baseline requirement. They automatically check for errors before submission, verify required fields, and flag payer-specific rules. These claims rejection management tools catch problems early when they are still easy to fix.
Real-Time Analytics
Analytics turn denial data into action. Teams can see which payers deny the most, which codes cause trouble, and whether appeals are working. Many platforms now combine real-time reporting with automated claims denial management features to reduce repeat issues.
AI, Automation, and Smart Appeals
Automation has changed the game. Some tools can identify a denial, attach missing documentation, and resubmit a claim with minimal human input. Others draft appeal letters tailored to the denial reason. Used correctly, this supports scalable claims denial management without sacrificing accuracy.
Reliable Outsourcing Partner
If you outsource, your partner should be using these tools too. At HelpSquad, denial specialists work with real-time dashboards and predictive insights to stop denials before they start. This approach works for large hospital systems and smaller practices alike.

People Still Matter in Claims Management
Specialized Denial Teams
Technology helps, but people still win appeals. Dedicated denial teams understand payer rules, coding logic, and appeal strategies. That expertise is hard to replace and critical for effective healthcare claims denial management.
Augmenting Your Team Through Outsourcing
Outsourcing does not replace your team. It extends it. HelpSquad provides trained denial specialists who plug into existing workflows. For smaller teams, this can feel like getting breathing room back.
Feedback Loops and Communication
Most denials trace back to front-end issues. That is why communication matters. Billing, front office, and clinical teams need feedback loops. When patterns show up, teams talk about them and fix the root cause. That is how hospital denials management best practices actually stick.
Never Stop Learning
Payer rules change. Codes get updated. Denial trends shift. Ongoing training is not optional anymore. Teams that invest in education consistently see lower denial rates over time.
Claim Denials You’ll Still See in 2025
Some denials refuse to go away. Common ones include:
- Missing or incorrect patient information
- Services without prior authorization
- Insurance eligibility issues
- Coding errors
- Insufficient documentation for medical necessity
- Late submissions
- Duplicate claims
Then there are payer policy changes that appear with little warning. These are easy to miss and costly if ignored. This is another reason outsourcing helps. RCM-focused partners track these changes closely.
Conclusion
If denials feel endless, you are not alone. The providers doing well in 2025 are not just reacting. They are investing in smarter claims denial management, prevention-focused workflows, and systems that improve over time.
“In healthcare, the experience of the patient is the new marketing.”
– David Feinberg, former CEO of Geisinger Health
If you are stretched thin or do not want to build a full in-house denial team, outsourcing is a practical move. HelpSquad gives providers access to experienced denial specialists, claims rejection management tools, automated claims denial management, and real-time insights that fit into daily operations. Talk to us.
FAQs
What is claim denial management?
Claim denial management is the process of identifying, correcting, appealing, and preventing denied insurance claims so providers can recover revenue and reduce future denials.
How do you handle claim denials?
Handling claim denials typically involves these key steps:
Identify and review the denied claim and the reason provided by the insurer.
Analyze the root cause of the denial using the payer’s explanation of benefits or reason codes.
Correct errors and resubmit the claim if appropriate.
Appeal the denial when possible, especially for complex issues like medical necessity.
Monitor and track denial patterns to prevent future occurrences.
What are the three types of claim denials?
Hard denials: Final denials that cannot be appealed or corrected.
Soft denials: Temporary denials that can be fixed and resubmitted.
Administrative denials: Denials caused by non-clinical issues like missing data or authorization errors.
What is the role of claims management?
Claims management oversees the full lifecycle of insurance claims, from submission to payment, ensuring accurate billing, timely follow-ups, and proper reimbursement.
How can you ensure that the information in this article is reliable?
This article is based on established healthcare revenue cycle practices and guidance from recognized industry organizations and payer documentation.


